What is Trichodysplasia spinulosa?
Trichodysplasia spinulosa is a rare skin condition that causes painless red bumps on the face with spiky, hair-like growths around the hair follicles. This condition occurs only in people who have a specific virus called trichodysplasia spinulosa-associated polyomavirus (TSPyV) and are also immunosuppressed, meaning their immune system is weakened.
This condition was first identified in 1995 and was believed to be a side effect of a drug called cyclosporin. However, further cases revealed that a weakened immune system, not the drug cyclosporin, is the common link between patients with this condition. In 1999, the condition was officially named ‘trichodysplasia spinulosa’ when it was found to be caused by a virus. In 2010, this virus was identified as a new type of virus, now known as trichodysplasia spinulosa-associated polyomavirus.
Continuous recognition and documenting of trichodysplasia spinulosa in medical research is necessary to improve our understanding and treatment of this rare condition.
What Causes Trichodysplasia spinulosa?
The Trichodysplasia spinulosa-associated polyomavirus (TSPyV) is a type of virus that comes from a family of viruses called Polyomaviridae. It falls under the Alphapolyomavirus group. In simpler terms, it’s also known as Human polyomavirus 8.
These polyomaviruses are really tiny, about 45 nanometers in size. To give you a sense of that size, a human hair is about 75,000 nanometers wide. These viruses carry a circular DNA structure inside a protective casing.
The name “polyomavirus” is made up of “poly,” which means multiple, and “oma,” which means tumor. This name hints at the ability of some types of these viruses to cause tumor formation in animals with weak immune systems.
In people, polyomaviruses are pretty common but usually do not cause any symptoms. However, when a person’s immune system is weakened, TSPyV can cause a condition called trichodysplasia spinulosa. This could be because of a new TSPyV infection, being exposed to the virus again, or the reactivation of a virus that was already present but inactive in the body.
Interestingly, despite many people carrying this virus, only a few people develop trichodysplasia spinulosa. This suggests that there might be other factors in play that we haven’t discovered yet.
Risk Factors and Frequency for Trichodysplasia spinulosa
Trichodysplasia spinulosa, although mostly observed in people with weakened immune systems, can happen in anyone as the virus causing it is widespread. Research shows that 65-80% of the population, even those with healthy immune systems, have the virus. There doesn’t seem to be a bias towards a certain gender, and the virus seems to infect people mostly during their childhood. But details about where it happens most are hard to find because the disease is rare and not reported often.
However, it may become more evident where this disease is most common as more cases get reported, and the disease becomes more recognized. Notably, these places might coincide with regions where there are more people with weakened immune systems.
There are certain factors that can increase the risk of getting trichodysplasia spinulosa. These include undergoing a solid organ transplant, taking drugs that suppress the immune system, having a blood-related cancer, and being infected with HIV. Almost all known cases occurred in patients who unquestionably had a compromised immune system.
Interestingly, there was one case in September 2014 where a man with Gorlin syndrome was being treated for multiple basal cell carcinomas with a drug called vismodegib, and he developed trichodysplasia spinulosa. This case was unusual because the disease caused him pain, and his condition improved once he stopped taking the medication. He had no prior instances of immune deficiency. Despite occasional outliers, most cases of trichodysplasia spinulosa are found in patients who have undergone solid organ transplants or have leukemia.
Trichodysplasia spinulosa is mostly seen in people with weak immune systems, but the virus that causes it is quite common. Even people with healthy immune systems can have the virus, and research shows that it’s present in 65-80% of the population. The virus seems to infect people in their childhood and doesn’t favor any gender. Since it’s a rare disease, there’s not enough data to show where it’s most common, but as it becomes more recognized and reported, we might start to see patterns.
There are a few things that can increase your chances of getting the disease. These include:
- Having a transplant of a solid organ
- Taking medication that weakens your immune system
- Having a blood-related cancer
- Being infected with HIV
Almost all known cases happened in patients who unmistakably had weak immune systems. There was one unusual case in 2014 where a man who was being treated for multiple skin cancers with a drug called “vismodegib” developed the disease. He didn’t have a history of immune deficiency, and his condition improved once he stopped the medication. Despite occasional unusual cases, most trichodysplasia spinulosa patients have either had a solid organ transplant or a form of leukemia.
Signs and Symptoms of Trichodysplasia spinulosa
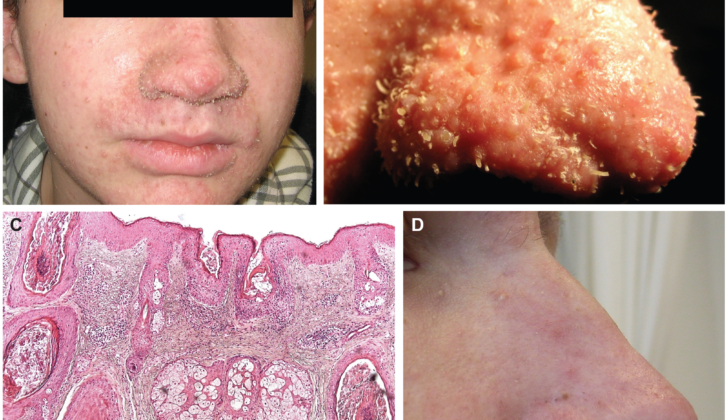
Trichodysplasia spinulosa is a condition that starts with a textured, bumpy rash on the face and a form of temporary eyebrow hair loss that doesn’t result in scarring. The skin changes, often called “spicules”, do not usually cause discomfort, but they can feel itchy. As these skin changes spread and the skin becomes thicker, they can alter the shape of the face, leading some to describe the look as “leonine” or lion-like. The color of these skin changes can vary—they could be the same color as the surrounding skin, red, or darker. While the skin changes are most often seen on the face, they can also appear in other areas, including the ears, the torso, and the arms.
Trichodysplasia spinulosa is typically seen in individuals who have a weakened immune system. This weakened state could be due to medications or specific conditions, such as following an organ transplant, while battling cancer, or living with HIV. It is most commonly reported in people who have had an organ transplant and are taking medications to prevent their bodies from rejecting the new organ, or in individuals who are undergoing treatment for blood or lymph system cancers.
Testing for Trichodysplasia spinulosa
: When your doctor suspects that you may have trichodysplasia spinulosa, a skin condition, they use several tools to confirm the diagnosis. They might take a small sample of your skin for a biopsy. This sample will be examined closely under a microscope, a process known as histopathological examination.
Two other key tools they might use are polymerase chain reaction like, or PCR, and electron microscopy. A blood test to check for the condition is usually not required but may be helpful, especially if you haven’t previously been diagnosed with an underlying condition that can weaken your immune system, such as HIV.
In the first of these tests, PCR, the doctor uses a small tissue sample taken from the affected area of your skin. This test looks for large numbers of the TSPyV virus in your tissue, a strong hint that you have trichodysplasia spinulosa. However, tests from unaffected areas or those showing low numbers of the virus are not very useful. This is because the TSPyV virus can be present in various types of tissue, even in individuals who show no signs of trichodysplasia spinulosa.
Electron microscopy involves looking closely at the affected tissue under a high-powered microscope. With this tool, doctors look for specific patterns suggesting trichodysplasia spinulosa, like clusters of viral particles with a distinctive “bumpy” appearance.
Even though blood tests are not always necessary in diagnosing trichodysplasia spinulosa, your doctor might still recommend some. As this skin condition can be linked to a weakened immune system, it might be useful to check for signs of conditions like HIV, by doing a test like a complete blood count or antibody titers. How much further to investigate this will depend on what your doctor thinks is best.
Treatment Options for Trichodysplasia spinulosa
Trichodysplasia spinulosa is a rare skin disorder, and finding an effective treatment has proven challenging. But currently, three approaches mark significant progress. These include the use of a skin cream called cidofovir, a medication named oral valganciclovir, and adjusting the body’s immune response (known as immunosuppression).
Many case reports suggest that cidofovir cream seems to show promising results when applied to the skin, making it a go-to treatment. Interestingly, the science behind this is that cidofovir can prevent the growth of a virus that’s thought to contribute to this condition. Another medication, oral valganciclovir, has also shown promising results in certain cases, and it’s easier to find than cidofovir cream. However, more research is needed to confirm its effectiveness against the virus.
Regarding adjusting the body’s immune response, it’s a delicate balance. While doing so could potentially reverse trichodysplasia spinulosa, it poses a risk of not getting enough of the patient’s regular immunosuppressive therapy, potentially leading to issues like the rejection of a transplant or the worsening of the underlying disease. Therefore, this approach should be taken with caution.
Additionally, various other skin treatments have been tried with mixed results. These include leflunomide (a medication used to treat autoimmune conditions), topical retinoids (medicines derived from vitamin A), steroids, imiquimod (a cream that stimulates the immune system), keratolytics (a type of skin treatment that can help with scaling), emollients (moisturizers), green tea extract, and other antiviral medications.
What else can Trichodysplasia spinulosa be?
To officially diagnose a condition known as Trichodysplasia spinulosa, two techniques can be used: studying the disease under a microscope (known as Histopathology) and conducting a type of DNA test known as Polymerase Chain Reaction. When doctors diagnose this disease, they need to also consider ruling out other conditions that may look similar:
- Trichostasis spinulosa: This disease is usually not associated with any symptoms and is characterized by skin changes involving an overgrowth of hair follicles.
- Follicular hyperkeratotic spicules: This condition is mostly linked with a blood cancer known as multiple myeloma and can be seen on the face.
- Lichen spinulosus: Featuring skin bumps and keratin spine development, this condition usually affects the trunk and arms/legs.
- Spiky follicular mycosis fungicides: Red, overgrown follicular skin bumps associated with lymphoma, a type of blood cancer.
- Disseminated spiked hyperkeratosis: Small, non-follicular keratin spikes with a genetic link.
- Ulerythema ophryogenes (keratosis pilaris atrophicans fasciei): A condition characterized by red facial bumps, eyebrow hair loss and scarring.
- Follicular-based graft versus host disease: A condition featuring overgrown, red follicular skin bumps which occur after a bone marrow transplant.
Additionally, doctors examine other types of polyomavirus of the skin that have been discovered – seven different species in total. Beyond Trichodysplasia spinulosa, this includes the Merkel cell polyomavirus and human polyomaviruses 6, 7, 9, 10, and 13. At this time, the Merkel cell polyomavirus as well as human polyomaviruses 6 and 7 have been found to cause diseases, especially in individuals with weakened immune systems. The Merkel cell polyomavirus, for instance, is known to cause a type of skin cancer. HPVy6 and HPVy7 are associated with itchy and abnormal skin growth, known as pruritic and dyskeratotic dermatosis. However, more case studies are needed to establish these characteristic presentations.
What to expect with Trichodysplasia spinulosa
Trichodysplasia spinulosa is a condition without a universally agreed upon treatment plan. However, the outlook for this condition is generally quite good, although full recovery may take anywhere from a few months to a few years. In some instances, the condition will improve on its own or after a patient completes treatment for a separate condition that weakens the immune system.
The associated loss of eyebrows and eyelashes, as well as changes to the face’s appearance, also tends to get better over time as the active disease resolves. That said, the underlying condition causing or requiring the suppression of the patient’s immune system plays a significant role in their overall prognosis or outlook.
Possible Complications When Diagnosed with Trichodysplasia spinulosa
Possible complications include itching, temporary loss of eyebrows and eyelashes, changes in facial appearance, and the resulting psychological stress these symptoms may cause.
Possible Complications:
- Itching
- Temporary loss of eyebrows and eyelashes
- Changes in facial appearance
- Resulting psychological stress
Preventing Trichodysplasia spinulosa
Patients should be comforted with the fact that trichodysplasia spinulosa, a skin condition that results in the growth of small, spiky hair, is harmless. Over time, with proper treatment and, if necessary, once immunosuppressive therapy (a treatment that reduces the body’s immune response) is complete, the changes in the skin will disappear, and the eyebrows will grow back. As of now, there isn’t a universal treatment for this condition, but applying “cidofovir” cream on the troubled skin area and taking “valganciclovir” orally or by mouth have shown successful results in many cases.