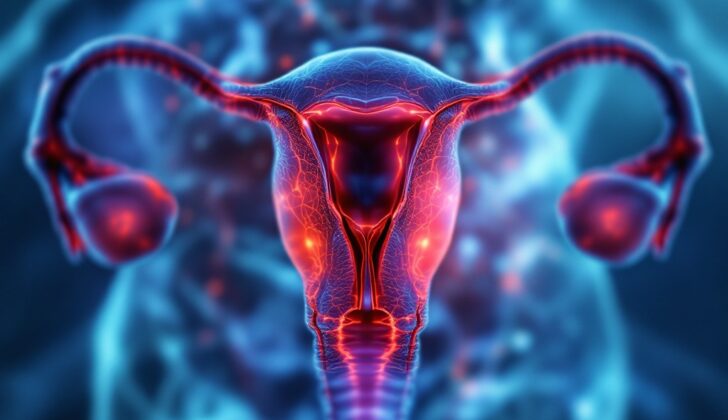
What is Endometrial Polyp?
Endometrial polyps are growths that develop on the lining of the womb or uterus. These growths can range in size from a few millimeters to several centimeters in diameter. There might be just one polyp or multiple ones filling up the whole space of the womb. While these polyps can be found at any age, women between the ages of 40 to 49 are most commonly diagnosed with it. Even though these polyps are usually non-cancerous, there is a slight chance they might turn into cancer.
What Causes Endometrial Polyp?
Endometrial polyps are abnormal growths that stick out from the endometrium, which is the lining of the uterus. We don’t know the exact causes of endometrial polyps, but they are often seen with a condition called endometrial hyperplasia. This is a thickening of the uterus lining and is often a result of too much estrogen in the body.
Other factors like increased enzymatic activity in the endometrium, certain proteins and genes are associated with polyp formation. There is also a connection between developing polyps and long-term use of a drug called tamoxifen, with 20% to 35% of women on the medication developing these overgrowths.
Mostly, these polyps are harmless, but some can potentially turn into cancer. The range of these becoming cancerous is between 0 and 13%. Factors like your age and whether you’ve reached menopause can increase the likelihood of polyps turning cancerous. For example, women over 60 and those who have reached menopause have a higher risk, especially if they experience bleeding or have another condition called polycystic ovarian syndrome. Women who have symptoms and have gone through menopause have a 4.47% chance of having cancerous polyps compared to a still high, but lower 1.51% chance in women who are asymptomatic.
Risk Factors and Frequency for Endometrial Polyp
Endometrial polyps can affect women of all ages, but they are most commonly seen in women aged 40 to 49. They are particularly associated with abnormal uterine bleeding. It’s estimated that 20 to 40 percent of women who experience this bleeding have endometrial polyps. Further, these polyps are found in roughly 10 percent of women during autopsy examinations. It’s important to note, though, that premenopausal women are less likely to have cancerous endometrial polyps than women who have gone through menopause.
- Endometrial polyps can happen at any age, but are most common in women aged 40 to 49.
- These polyps are found in 20 to 40 percent of reproductive-aged women who have abnormal uterine bleeding.
- About 10 percent of women are found to have these polyps during an autopsy.
- Premenopausal women are less likely than postmenopausal women to have cancerous endometrial polyps.
Signs and Symptoms of Endometrial Polyp
Endometrial polyps are medical conditions which some patients may not show any signs of, or they may experience abnormal uterine bleeding. This bleeding is the most common symptom. Other symptoms might include pain in the stomach or pelvis, or difficulty getting pregnant. It’s important to note that one in four women in their childbearing years who have abnormal bleeding will also have endometrial polyps.
Part of diagnosing endometrial polyps involves understanding if there are other symptoms and any related conditions. It’s critical to take a thorough look at a patient’s medical history and past surgeries to rule out other causes of abnormal uterine bleeding. Interestingly, there isn’t a specific bleeding pattern for endometrial polyps, but the most commonly reported ones are heavy menstrual bleeding and spotting in between periods.
Some drugs, such as Tamoxifen, which is commonly used to treat breast cancer, may also have a role in the development of endometrial polyps. While Tamoxifen works against cancer in breast tissue, it could potentially lead to cancer in endometrial tissue. Chronic use of Tamoxifen has been connected with the development of endometrial polyps in 20% to 35% of cases. Similarly, hormone replacement therapy, used to manage symptoms of menopause, may also be linked to the formation of endometrial polyps. The usual symptoms related to this are irregular bleeding and a thickened lining of the uterus as seen in an ultrasound.
During a visit to the clinic, a general physical exam, as well as a two-handed examination and a speculum exam (which helps a doctor see inside the vagina), should be conducted. The cervix and the upper part of the vagina need to be thoroughly checked to rule out other structural causes for the symptoms. In some cases, an endometrial polyp that has grown into the cervical canal may be seen from the opening of the cervix.
Testing for Endometrial Polyp
Transvaginal ultrasound is a common and effective method to create images of pelvic structures. With this technique, the lining of the uterus, or endometrium, may show up as thicker on ultrasound. This is not specific to any one condition and could be seen in many situations. In women who have bleeding after menopause, a thickness of less than 4 mm usually means the lining of the uterus is getting thinner or atrophic. But, if this thickness is greater than 4 mm, it might suggest problems such as tissue growths called polyps. The position, number, and size of these polyps does not necessarily correspond with the symptoms reported.
One other way to examine the uterine cavity is through a procedure called saline-infusion sonography (SIS). In this method, a small quantity of warmed saline water (about 5 to 30 mL) is injected into the uterus using a thin tube during certain phase of menstrual cycle. The fluid helps detect polyps by outlining them. This procedure should not be performed in cases of active uterine or cervix infection and pregnancy. Compared to transvaginal ultrasound, SIS gives a better view of the corners of the uterus and adnexa, and also distinguishes better between submucosal fibroids and endometrial polyps by observing their location relative to the uterus lining. A polyp will be seen coming from, or arising from the endometrial layer, while a fibroid will be seen under this layer. Other techniques for examination include hysterosalpingograms or hysteroscopy.
However, it’s important to note that these methods don’t provide tissue samples for detailed medical examination. Because there’s a risk of cancer associated with endometrial polyps, getting a tissue sample should be considered. To do this, an endometrial biopsy, dilation and curettage (D&C), or hysteroscopic polypectomy would be necessary. Traditional tissue sample collection with endometrial biopsy or D&C without visualization is not very accurate in diagnosing endometrial polyps and should be used only when hysteroscopic treatment is not available.
Lab examinations are also an important part of evaluating abnormal uterine bleeding. These tests might include a urine pregnancy test, a complete blood count, and a panel to check for any clotting disorders to rule out conditions such as anemia and coagulopathy, which affect the blood’s ability to clot.
Treatment Options for Endometrial Polyp
If you’re a patient with no symptoms and a low risk, doctors usually observe and monitor endometrial polyps rather than immediately treating them. Endometrial polyps are tissue growths in the lining of your uterus, and they could disappear on their own without treatment. One study found that 29% of these polyps disappeared naturally within a year in patients before menopause. If you’re under regular observation, the doctor uses ultrasound to keep track of the polyp’s size.
Some doctors might suggest hormonal therapy, but there isn’t enough medical research to fully support this treatment right now. Mostly, the preferred treatment for an endometrial polyp is a procedure called hysteroscopic polypectomy, which is the removal of the polyp. These polyps sometimes harbor underlying uterine abnormalities, such as endometrial carcinoma (a type of cancer), so it’s important to test the polyp and the surrounding tissue to investigate further. Polyps disappear in about 20% of the cases following this type of cancer diagnosis.
However, the timing of when to perform a polypectomy isn’t cut and dried, particularly for asymptomatic or low-risk individuals. One study of asymptomatic women concluded that it’s unclear when polypectomy should be performed routinely as no cancer was found on the removed polyps. It’s important to note that larger polyps (more than 1.5 cm in length) are less likely to disappear on their own and removal may be considered, especially if they cause symptoms.
Hysterectomy, which is the removal of the uterus, is a more extreme surgical option that effectively eliminates the chance of polyp recurrence and the potential for malignancy. However, because it’s a major procedure, the risks to the patient and the costs associated are significant. A hysterectomy should only be considered after the patient is thoroughly informed about the implications.
If you’re experiencing anemia due to abnormal bleeding from your uterus, your doctor might recommend taking daily iron supplements.
What else can Endometrial Polyp be?
When a diagnosis is being conducted, several possible conditions could be considered. These include:
- Submucosal leiomyoma (a type of tumor in the uterus wall)
- Adenomyoma (a noncancerous growth of the uterus)
- Retained products of conception (remaining tissue after pregnancy)
- Endometrial hyperplasia (a condition where the lining of the uterus becomes too thick)
- Endometrial carcinoma (cancer of the uterus lining)
- Uterine sarcomas (a rare type of cancer that starts in the muscle and supporting tissues of the uterus)
What to expect with Endometrial Polyp
After a surgery known as hysteroscopic polypectomy which is used to remove polyps from the uterus, it has been reported that bleeding between menstrual cycles often lessens significantly. The treatment tends to be effective with a low chance of the polyps returning, especially in patients who initially had fewer polyps. The recurrence rate for polyps that are confirmed through lab testing is around 2.5% to 3.7%.
If this polyp removal surgery is combined with endometrial ablation (a procedure that destroys a thin layer of the lining of the uterus) or the insertion of a levonorgestrel-releasing intrauterine device (a type of birth control that is placed inside the uterus), the chances of the polyps coming back might be reduced even further. However, data to support these treatments is somewhat limited, which means they’re typically only currently used in research contexts.
If polyps are linked with the use of tamoxifen, a medication used to treat breast cancer, an intrauterine device (IUD) that releases levonorgestrel (a hormone) has been found to potentially help prevent new polyps from forming and could be a useful part of treatment plans.
In addition, there are some studies showing rates of natural pregnancy and full-term births increased after the removal of polyps through hysteroscopic polypectomy. Importantly, there doesn’t seem to be any noticeable difference in the fertility rates between patients who had smaller polyps (1 cm or less) and those with larger or multiple polyps. Also, having smaller or larger/multiple polyps did not seem to affect the rate of miscarriage in the first trimester of pregnancy.
Possible Complications When Diagnosed with Endometrial Polyp
After a procedure to remove polyps from the uterus using a small camera (hysteroscopic polypectomy), the removed specimens are sent for medical testing to check whether they are potentially harmful. If the polyps show signs of cancer, the next step would be a referral to doctors specializing in women’s cancer care (gynecology oncology). Luckily, complications from the polyp removal procedure are uncommon, and the risk of scar tissue forming inside the uterus is low.
There are different opinions in the medical community about whether there’s a link between polyps in the womb (endometrial polyps) and the risk of not being able to have children (infertility). One reason for this is based on a study where the chances of becoming pregnant improved after removing womb polyps before intrauterine insemination – a medical procedure to assist pregnancy. Moreover, womb polyps are more common in patients who can’t conceive due to blocked fallopian tubes.
However, another study showed that pregnancies via in-vitro fertilization – another medical procedure to help with pregnancy – did not change whether patients had known polyps during the process. This study also showed no difference in rates of miscarriages or living births. Despite these differing studies, medical experts tend to recommend removing womb polyps before attempting in-vitro fertilization.
Preventing Endometrial Polyp
It’s necessary to educate patients on the causes and ways of managing abnormal uterine bleeding. Most uterine polyps, which can contribute to this bleeding, are not dangerous, but there is a small chance they could turn into cancer. The mention of cancer can be mentally distressing, so this is a delicate topic that needs to be handled carefully. Uterine polyps can also affect a patient’s quality of life and the ability to have children in the future.
Patients should also understand that polyps can come back and there are specific lifestyle changes that can help reduce this risk.