What is Procidentia?
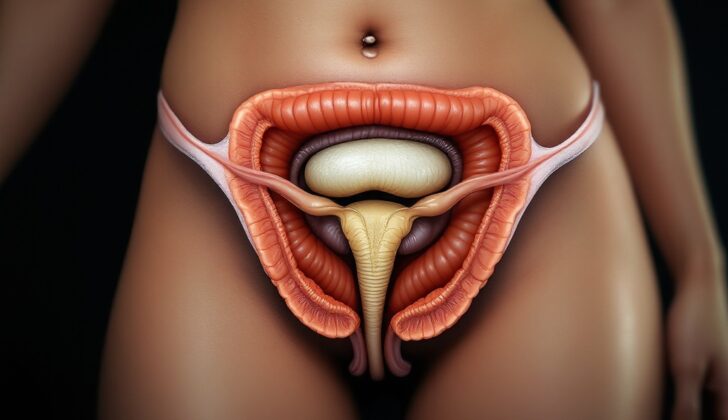
Procidentia is a serious condition where the organs in the pelvis such as the vagina, intestine or uterus, slide out of place and protrude through the vaginal opening. This can affect either individual parts of the pelvic area or the entire area, as happens in procidentia. Specifically, when the front of the vagina protrudes it’s called a cystocele, when the back of the vagina protrudes it’s a rectocele, and when the top part of the vagina protrudes, it can either be bowel (enterocele) or uterus (uterovaginal prolapse).
The first known record of pelvic organ prolapse dates all the way back to 1550 BC, found in an ancient Egyptian medical text called Ebers Papyrus. Over time, people have tried various ways to treat it – from manually pushing the organs back into place, to cleaning the protruding organ with oils and wines, and even inhaling unpleasant smells. One particular method was called “succession”, where women were turned upside down on a ladder and shaken in the hopes that gravity would pull the organs back into their normal position. At times, early forms of surgery were performed to remove the uterus. This method, known as a vaginal hysterectomy, was first documented in the early 16th century by a physician named Capri, who performed it as a treatment for pelvic organ prolapse.
While prolapse often doesn’t cause pain or threaten one’s life, it can significantly affect daily activities, self-image, and sexual health. The desperation caused by this condition can be seen in a historical account from the 17th century, where a woman who was unable to seek medical help, tragically attempted to remove her prolapsed uterus by herself. She assumed it was a growth from her vagina and cut it out, which caused heavy bleeding that eventually stopped. However, she likely developed a vesicovaginal fistula, a type of abnormal passage between the urinary bladder and the vagina, which led to issues with urinary incontinence.
Fortunately, in the 19th and 20th centuries, advances in surgical tools, anesthesia and antibiotics have made surgeries like hysterectomies much safer and less likely to lead to complications. Many different treatment options for pelvic organ prolapse are now available.
What Causes Procidentia?
Pelvic organ prolapse can be caused by many medical conditions and risk factors. Some of these are changes in the structure of the pelvic region, like if the uterus becomes enlarged because of conditions like leiomyoma (noncancerous growths in the uterus) and endometriosis (a condition where tissue similar to the lining of the uterus grows outside of the uterus). Pregnancy and childbirth through the vagina have also been linked to pelvic organ prolapse.
Factors outside the body, like smoking and obesity, have also been listed as risk factors for pelvic organ prolapse. Remember that these factors increase the chances of experiencing pelvic organ prolapse but do not guarantee it will happen.
Risk Factors and Frequency for Procidentia
The Women’s Health Initiative Hormone Replacement Therapy clinical trial identified a group of older women with pelvic organ prolapse. The exact prevalence of this condition is unclear, as categorization methods vary and many women do not initially seek medical help for prolapse.
- About 1 in 10 women will need surgery for pelvic organ prolapse by the age of 80.
- The prevalence of surgery for this condition varies between 6% and 18%.
- Based on symptoms, the prevalence of pelvic organ prolapse ranges from 3% to 6%,
- By means of vaginal examination, this percentage could be as high as 50%.
There’s a general agreement in many studies that pelvic organ prolapse should have a more exact classification system. This would aid in better understanding and researching this condition.
Signs and Symptoms of Procidentia
Pelvic organ prolapse often develops gradually and is commonly noticed as a feeling of fullness or bulge in the vagina. This symptom might be discovered by chance during regular gynecological check-ups. People with this condition should also be evaluated for other issues related to the female urinary and reproductive system.
It’s important to note that some people with prolapse might also have other problems such as:
- Stress urinary incontinence (found in 40% of cases)
- Overactive bladder (found in 37% of cases)
- Fecal incontinence (found in 50% of cases)
People may notice changes in their symptoms throughout the day. For instance, the bulging sensation may not be as noticeable when first getting up in the morning, but can worsen with activity like lifting, straining, or standing for long periods. It’s also possible to experience skin irritation and tissue damage when the internal vaginal lining is exposed due to severe uterine prolapse (procidentia).
Testing for Procidentia
The diagnosis of a condition called prolapse is typically made through a physical examination. The need for laboratory tests or imaging like X-rays or scans is not common for this condition.
Since 1996, significant medical societies such as the International Continence Society, the American Urogynecologic Society, and the Society of Gynecologic Surgeons have been using a specific system called the Pelvic Organ Prolapse Quantification system (POP-Q) to examine and diagnose prolapse. Before this, other methods were used for evaluation.
Even though the POP-Q system is a bit complex to learn, it is a reliable examination that is widely used in medical and research practices. There are five stages of prolapse, which this test helps to identify, based on measurements of specific points of the vaginal vault in relation to the hymen. The hymen is a thin piece of tissue that surrounds or partially covers the external vaginal opening.
Here are the five stages:
– Stage 0 – No signs of prolapse
– Stage 1 – The furthest point of the prolapse is more than 1 cm above the hymen level
– Stage 2 – The furthest point of the prolapse is between 1 cm above and 1cm below the hymen level
– Stage 3 – The furthest point of the prolapse is more than 1 cm below the hymen, but not completely turned inside out
– Stage 4 – The uterus is entirely turned inside out
A stage 4 prolapse is also known as procidentia. Most women who experience symptoms from their prolapse usually have a prolapse at stage 2 or higher.
Treatment Options for Procidentia
Prolapse, which includes a condition known as procidentia, is not life-threatening. The severity of the person’s symptoms guides the treatment. If someone is diagnosed with prolapse but doesn’t have any symptoms, monitoring the condition and doing exercises to strengthen the pelvic floor muscles can be appropriate options. However, there’s no guarantee that the prolapse will get better, stay the same or get worse over time.
For those who do have symptoms but don’t want surgery or aren’t suitable candidates for surgery, pessaries might be a good alternative. Pessaries are often made of silicone and come in a variety of sizes and shapes. They are designed to suit a person’s specific type of prolapse. They are used by different people, including women who wish to have children in the future but are experiencing symptoms of prolapse, or elderly women who have other health conditions that make the use of anesthesia risky.
Surgical treatment options can depend on many factors. These include the stage of the prolapse, the length of the vagina, hormonal status, whether the person wants to have sex in the future, and whether there are any other urinary or bowel problems. Various studies have compared different surgical techniques for repairing the pelvic floor. An extensive study involving women aged 70 to 80 who requested surgery showed that three methods—sacrocolpopexy, native tissue repair, and vaginal mesh repair—had comparable recovery times, success rates, and patient satisfaction levels.
The International Federation of Gynecology and Obstetrics has looked at various surgical procedures and compared their effectiveness alongside their cost. Pessaries had the lowest complication rate and were the most cost-effective. In terms of vaginal surgeries, sacrospinous ligament fixation and uterosacral ligament suspension had similar results. For abdominal surgeries, a minimally invasive approach called sacrocolpopexy was found to be durable, improve quality of life, and have the least amount of complications.
What else can Procidentia be?
If a patient shows signs of pelvic organ prolapse, doctors can usually identify this during a physical examination. Nevertheless, before planning treatment, certain accompanying conditions may need to be investigated. These typically involve gaining a thorough understanding of the patient’s history related to bladder, bowel, and sexual symptoms.
What to expect with Procidentia
Procidentia, or complete uterine prolapse, generally has a good prognosis, meaning it’s not a life-threatening condition and can be treated effectively. Rather than physical health, it mostly impacts quality of life, and this is typically the main reason why most women seek treatment.
Initial treatment usually aims to slow down the progression of the prolapse, using non-surgical methods. A popular non-surgical treatment involves the use of devices known as pessaries. These are particularly beneficial for post-menopausal women with severe prolapse, as they can significantly improve quality of life and reduce the symptoms associated with vaginal prolapse.
Moreover, several studies have reported that surgical interventions for pelvic organ prolapse, including procidentia, not only provide immediate relief but continue to improve the quality of life and patient satisfaction for an average of two to five years after the surgery.
Possible Complications When Diagnosed with Procidentia
Prolapse, which is a health condition where organs slip out of their usual position, can interfere with bladder function, bowel movements, and even sexual health.
Before any surgery, doctors can perform bladder trials involving simple tests to predict potential post-surgery incontinence, or a loss of bladder control. This tends to occur as a result of the bladder returning to its normal position after the prolapse is treated. Regardless of whether or not the woman is currently experiencing bladder control issues, it’s still recommended to conduct a bladder test in women with this condition. This helps doctors decide whether surgery for incontinence is needed at the same time.
Bowel complications may include either faecal incontinence or difficulty with bowel movements. Sometimes, patients report having to push on the wall of their vagina or perineum to assist bowel movements. This action, called ‘splinting’, is often due to a weakness in the pelvic ligaments or damage to connective tissue which affects the normal opening and closing of the anus.
Sexual health can also be impacted by prolapse. Even though the prolapse itself should not cause pain, it often induces negative feelings about one’s body. This can lead to problems in a woman’s sexual health due to embarrassment. It can also interfere with professional activities, as women may need to change or stop their activities due to discomfort.
Common Issues Related to Prolapse:
- Potential bladder control issues after surgery
- Fecal incontinence or difficulty with bowel movements
- The need to perform ‘splinting’ during bowel movements
- Negative impact on sexual health and body image
- Interference with professional activities due to discomfort
Preventing Procidentia
Several organizations, such as the International Urogynecological Association (IUGA) and the American Urogynecologic Society (AUGS), develop educational materials to help patients understand more about urogynecological health. These materials provide information about various tests and surgeries related to the female urinary and reproductive systems. In addition to this, patients are often given written instructions about pessaries, which are devices inserted into the vagina for support or to deliver medication. Having both written instructions and face-to-face consultations can help enhance patients’ confidence in managing their own care, such as the use of pessaries. This approach is useful because it lessens vaginal discharge and odor, as well as minimizes the time needed for routine follow-up care at the doctor’s office. Furthermore, there are visual aids designed to help patients understand more about surgeries for conditions like pelvic organ prolapse, which is when the pelvic organs drop due to loss of support. However, while these visual aids have been used to aid in the process of obtaining consent for surgery, they haven’t been shown to be more effective than only using verbal consent.