What is Tubo-Ovarian Abscess?
A tubo-ovarian abscess (TOA) is a serious infection that causes a lump in the adnexa, the area of a woman’s body that houses the ovaries and fallopian tubes. It’s typically a complication of pelvic inflammatory disease, an infection that affects a woman’s reproductive organs. Common symptoms include having a fever, high white blood cell count (which signals an infection), pain in the lower abdomen or pelvis, and/or unusual vaginal discharge. But the symptoms can vary a lot, making it hard to detect sometimes. If the abscess bursts, it can cause a dangerous, potentially life-threatening infection that spreads throughout the body (sepsis). That’s why it’s crucial that any suspicion of this condition be checked out and treated promptly.
Mostly, TOA affects women during their childbearing years, particularly those who are sexually active.
What Causes Tubo-Ovarian Abscess?
Abscesses, which are pockets of pus, can often occur as a late result of an infection called pelvic inflammatory disease (PID), which involves inflammation in the female reproductive organs. This typically starts as an infection in the cervix or vagina, which then spreads upwards into the lining of the uterus (endometrium), and then further still through the fallopian tubes. Once they’ve reached the area inside the abdomen (peritoneal cavity), they create a blocked-off mass. Most of these cases are also associated with inflammation of the lining of the abdomen, known as peritonitis.
These pockets of pus, or abscesses, can also occur due to an infection spreading from a nearby organ (most commonly the appendix), or from an infection somewhere else in the body, known as hematogenous spread. They can also be associated with cancer in the pelvic organs.
Risk factors for developing an abscess are similar to those for PID and include being of childbearing age, having an intrauterine device (IUD) inserted, having multiple sexual partners, and having had PID before. Many conditions can have similar symptoms to an abscess, making it tricky to diagnose. These usually include appendicitis, diverticulitis, inflammatory bowel disease, PID itself, twisted ovary (ovarian torsion), pregnancy outside the uterus (ectopic pregnancy), ruptured ovarian cyst, kidney infection (pyelonephritis), and bladder inflammation (cystitis).
Risk Factors and Frequency for Tubo-Ovarian Abscess
These abscesses, known as TOAs, are most often found in women of reproductive age who have had an infection in the upper genital tract. However, these abscesses can also occur without any previous infection or sexual activity, and can even develop as a complication of a hysterectomy.
In the past, nearly a fifth of the hospitalised cases of PID, a type of genital infection, were found to have a TOA. However, in 2002, new guidelines for the evaluation and treatment of sexually transmitted diseases were released by the CDC. As a result, more people started to get diagnosed with and treatment for PID. This has led to a significant decrease in the prevalence of TOA to just about 2.3%.
It’s worth noting that HIV positive women with PID tend to recover from the infection more slowly. This slower recovery puts them at a higher risk for developing a TOA.
Signs and Symptoms of Tubo-Ovarian Abscess
A tubo-ovarian abscess (TOA) typically shows up with symptoms like belly pain, a noticeable lump in the pelvic area during a physical examination, fever, and a high white blood cell count, which suggests an infection. However, it’s important to note that not everyone shows these typical symptoms. Some women might not have a fever and their white blood cell count could be normal. Only half of the women with a TOA come in with a fever and chills. Others might report different symptoms like a discharge, feeling sick to their stomach, or abnormal bleeding.
If a TOA is suspected, it’s crucial to start testing right away. The checks include a comprehensive physical and pelvic examination. This looks at important aspects like the feel, size, and flexibility of the womb and both ovaries. When there’s a thick pus-like discharge and pain when the cervix is touched, these are hints of pelvic inflammatory disease (PID). If there’s tenderness in the womb or ovaries, it raises concerns about a TOA. A detailed check of the abdomen and key signs like temperature, heart rate, and blood pressure will help understand the severity of the inflammation and the body’s overall response.
Doctors will also run routine blood tests to look for a high white blood cell count, and take samples for urine, cervical and blood cultures. Another test they might do involves looking at a drop of vaginal discharge under a microscope for “clue cells,” which suggests bacterial vaginosis. A pregnancy test is also mandatory, to rule out pregnancy in the womb or elsewhere.
Testing for Tubo-Ovarian Abscess
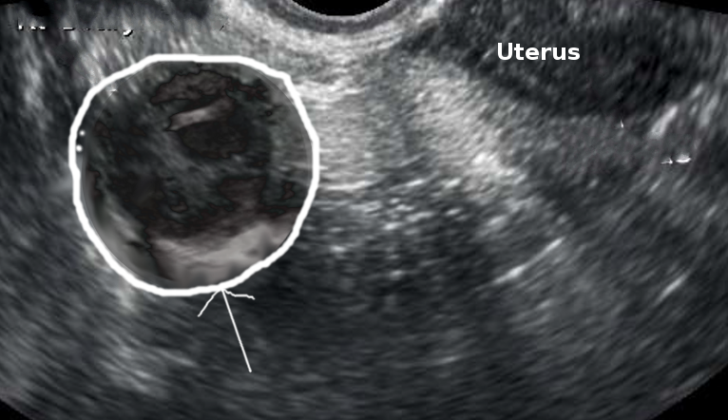
A tubo-ovarian abscess, or TOA, is a pus-filled pocket that involves a woman’s fallopian tube and ovary. It’s one of the late complications of pelvic inflammatory disease (PID). When a doctor suspects a TOA, they use certain imaging techniques to take a closer look at the ovaries. These techniques include sonography (an imaging technique that uses high-frequency sound waves), computed tomography (CT, a special type of x-ray imaging), or magnetic resonance imaging (MRI, a technique that uses magnetic fields and radio waves).
Studies have shown that MRI tends to be superior in evaluating the details of the disease and identifying a TOA. While MRI is a very accurate method, laparoscopy (a surgical procedure that allows a doctor to look inside the body using a thin, lighted tube) is still considered the best way to diagnose PID and TOA. A laparoscopy can also help drain the abscess and collect a sample for testing.
Usually, either a transvaginal ultrasound (where an ultrasound device is inserted in the vagina to get a closer look at the ovaries) or a CT scan of the abdomen and pelvis is used to investigate a suspected TOA. CT scans have shown a higher probability of detecting TOAs compared to ultrasounds. However, because ultrasounds are more affordable and do not expose the patient to radiation, they are often the preferred method for women who can still have children. In fact, one study found that ultrasound correctly identified TOA in 90% of those cases later confirmed by surgery.
When using a CT scan to image a TOA, doctors look for specific signs such as a thick, uniformly enhancing wall of the abscess, often with multiple compartment-like spaces and dense fluid within them. On an ultrasound, the normal structure of the fallopian tubes and ovaries is distorted. The wall of the fallopian tube appears thicker than normal (more than 5 mm), there is fluid in the cul-de-sac (a space in the lower abdomen), and there are incomplete walls inside the fallopian tube. A TOA typically appears as an intricate, multi-compartment mass containing echoes that are consistent with inflammation debris.
Treatment Options for Tubo-Ovarian Abscess
In the past, tubo-ovarian abscesses (TOAs), which are a serious complication of pelvic inflammatory disease, were typically treated with surgery to remove the uterus and both fallopian tubes and ovaries. However, treatment approaches have changed dramatically due to the introduction of broad-spectrum antibiotics, improved imaging techniques, and new methods of draining the abscess. Nowadays, many of these abscesses, about 70% or more, can be successfully treated even without surgery.
If a woman is found to have a TOA, she should be hospitalized and a specialist in women’s health (a gynecologist) should be consulted. If the abscess is detected before it bursts, treatment can usually start with a course of antibiotics given directly into a vein (intravenous, or IV). In one study, only about a third of patients who received this antibiotic therapy ended up needing surgery later on.
In general, treatment often starts with antibiotic therapy, with surgery reserved for cases where the abscess might have burst or when the abscess doesn’t respond to antibiotic treatment. One study showed that the size of the TOA can affect how successful medical treatment is. Abscesses larger than 10 centimeters were more likely to need surgery.
The Centers for Disease Control and Prevention (CDC) provides treatment guidelines for pelvic inflammatory disease (PID), which also work well for TOAs. These guidelines often include the use of an antibiotic called metronidazole or another called clindamycin, because they are both very good at treating the type of bacteria that can live without oxygen (anaerobic bacteria) and can penetrate the wall of the abscess. Clindamycin, in particular, is so effective that one study found 68% of patients treated with it saw a decrease in the size of their TOA.
Women with a TOA should receive antibiotics until their pain and tenderness have reduced significantly, they no longer have a fever, their white blood cell count is back to normal, and the size of the mass has either stabilized or decreased. Once these improvements are noted, the antibiotics can be switched to a form that can be taken orally, until imaging studies confirm the TOA has completely resolved.
If a patient’s symptoms get worse or if imaging studies show the TOA is getting bigger or it has ruptured, the treatment includes a full day of intravenous antibiotics in the hospital, followed by surgery to remove the abscess as well as the affected ovary and fallopian tube. After being discharged from the hospital, the patient will continue taking oral antibiotics until the infection is cleared.
Transvaginal ultrasound-guided aspiration with antibiotics – a procedure where a thin needle is inserted, guided by an ultrasound, to drain the TOA – has also shown to be a very successful treatment method. In one study, 93.4% of women who underwent this procedure along with antibiotics had a successful recovery, with over half experiencing complete pain relief within 48 hours of the first drainage. Results were so positive that the authors proposed this method could be considered as a first-line treatment.
In terms of surgical treatment, the infection can be managed through a number of ways, including a minor surgical procedure using a thin tube with a camera (laparoscopy), a major open surgery (laparotomy), draining the abscess, and removal of the fallopian tube. However, in today’s practice, most patients can be managed with a procedure to drain the abscess guided by imaging techniques.
At this point in time, though, there are no large-scale studies that give us a definitive answer on the role of these imaging-guided drainage procedures in the treatment of TOAs. As a result, the choice of whether to use surgery or imaging-guided drainage should be made on a case-by-case basis and depend on the expertise available.
What else can Tubo-Ovarian Abscess be?
These are some conditions that can cause similar symptoms and need to be considered when diagnosing a patient:
- Renal stone (kidney stone)
- Appendicitis (swelling of the appendix)
- Cholecystitis (inflammation of the gallbladder)
- Inguinal hernia (a condition in which internal parts of the body push through a weakness in the muscle or surrounding tissue wall)
- Obturator hernia (a rare type of hernia in the pelvic area)
- Bowel obstruction (a blockage of the intestines)
What to expect with Tubo-Ovarian Abscess
Most patients can be treated with antibiotics and a type of treatment called percutaneous drainage, which involves removing fluid from a body cavity or space using a needle. However, this recovery process can take some time. These patients often need to stay in the hospital and receive antibiotics through an IV.
Even after recovery, some people may continue to experience long-term pain in their lower abdomen, known as chronic pelvic pain. Additionally, these individuals may also have an increased risk of ectopic pregnancies, which are pregnancies that occur outside of the uterus and can be life-threatening if not treated promptly.
Possible Complications When Diagnosed with Tubo-Ovarian Abscess
Chronic pelvic pain is an issue that my persist after the procedure. In addition, the surgery may result in a distortion of the pelvic anatomy. There are also risks of complications if the woman decides to get pregnant in the future. This is because the surgery may increase the likelihood of an ectopic pregnancy. Furthermore, the procedure may cause fertility issues, making it more difficult for the woman to conceive. Lastly, there’s a risk of experiencing recurrent Pelvic Inflammatory Disease (PID), which is a condition where the female reproductive organs become inflamed.
Common Side Effects:
- Chronic pelvic pain
- Changes in the structure of the pelvic area
- Risk of ectopic pregnancy
- Possibility of infertility
- Recurring episodes of PID