What is Uterine Prolapse?
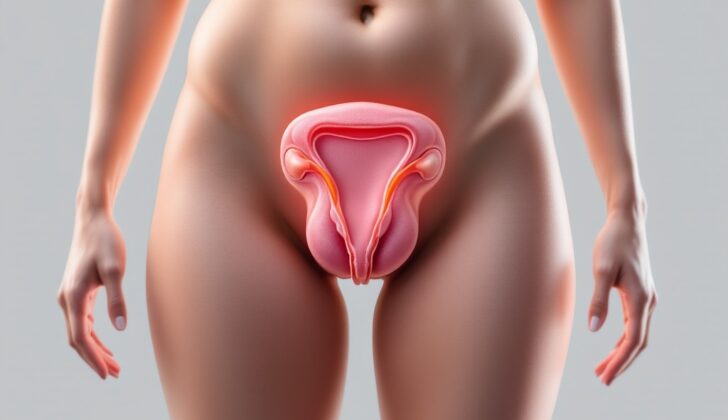
Uterine prolapse is a condition where the uterus, which is typically located in the pelvic region of the body, slips down into the vaginal canal. This can happen when the supporting structures around it become weak. Uterine prolapse is one of several conditions classified under the larger term of pelvic organ prolapse. This summary will explain the causes, how it’s diagnosed, and how it’s treated, as well as the role of healthcare providers in helping patients with this condition.
Under normal conditions, the uterus is positioned in the upper part of the pelvic organs. It’s held in place by ligaments, similar to strong, supportive bands, which connect it to the sacrum (part of the lower back) and the sides of the pelvis. When these ligaments become weak, the uterus can drop into the vaginal vault (the expanded part of the vagina). Even though uterine prolapse is not directly life-threatening, it can lead to issues such as sexual dysfunction, poor body image, and a lower quality of life due to things like bowel or bladder incontinence (the loss of control over one’s bowel or bladder).
What Causes Uterine Prolapse?
Uterine prolapse, where the womb slips down into the vagina, has the same risk factors as slippage of other pelvic organs. A study by the Oxford Family Planning Association found that women were more likely to experience such slippages, including uterine prolapse, with each subsequent childbirth.
Women who have a Body Mass Index (BMI) more than 25 have a greater chance of getting a uterine prolapse than women who have normal BMI ranges. BMI is a measure used to determine if you’re a healthy weight for your height.
There’s also a strong relationship between getting older and the occurrence of prolapses. So, as a woman ages, the chances of experiencing uterine prolapse gets higher.
Furthermore, people with connective tissue disorders, such as Marfan and Ehlers-Danlos syndrome, also have a higher risk. These are conditions that cause the tissues holding various parts of the body together to weaken.
Risk Factors and Frequency for Uterine Prolapse
Understanding the rates of uterine prolapse can be tricky, mainly because lots of studies mix it up with another condition called pelvic organ prolapse. An important study of 1961 women showed that pelvic organ prolapse affected close to 10% of women who are between 20 and 39, and almost half of women over 80 years old. So, we can say that about half of the women in the US might experience some pelvic organ prolapse as they grow older.
In developing countries like Nepal, the numbers are also significant. Out of approximately 15 million women, more than 1 million have been found to have uterine prolapse. This means that around 7% of women in Nepal are affected by this condition.
- About 10% of women from 20 to 39 years old, and almost half of the women over 80 suffer from pelvic organ prolapse.
- About half of the older women in the US might be expected to have some degree of this condition.
- In Nepal, more than 1 million out of around 15 million women have uterine prolapse.
- This equates to about 7% of the female population in Nepal.
Signs and Symptoms of Uterine Prolapse
Uterine prolapse, a condition in women where the uterus descends into or protrudes out of the vagina, often starts with the feeling or sight of a bulge in the vaginal area, coupled with a sensation of pressure. Other symptoms can include a frequent urge to urinate, feeling like the bladder isn’t entirely empty, and pain during sexual intercourse. However, it’s important to note that these symptoms usually start slowly and can intensify as the condition worsens. It’s also been noted that the severity of these symptoms may increase as the prolapse gets worse.
That said, the particular symptoms a woman experiences do not always directly mirror the severity or stage of the prolapse. In fact, in the early stages of uterine prolapse, many women do not show any symptoms at all.
Alongside the symptoms reported by the patient, a pelvic exam for direct visualization of the prolapsed portion is an integral part of diagnosing this condition. This involves checking the patient both while she is at rest and when she’s performing the Valsalva maneuver (a technique where the patient is asked to bear down as if having a bowel movement). The visibility of the prolapsed segment with respect to the hymen or introitus (the vaginal opening) during this exam is then used for staging the prolapse.
Testing for Uterine Prolapse
There are no specific lab tests that can help in identifying uterine prolapse, a condition where the uterus drops into or protrudes out of the vagina. The best way to diagnose this condition is mainly through a thorough review of your medical history and a pelvic exam performed by your doctor.
However, if your doctor needs more information, they might use imaging tools to get a clearer picture of what’s happening inside your body. These can include ultrasound (which uses sound waves to create a picture), CT scans (which use a series of X-ray images), and MRI (which uses magnetic fields and radio waves). These tests can help confirm the diagnosis.
Treatment Options for Uterine Prolapse
The treatment of uterine prolapse, a condition where the uterus slips from its normal position, often depends on how severe a patient’s symptoms are. Gentle approaches can include pelvic floor muscle training, which are exercises to strengthen the muscles that support the uterus, and the use of vaginal pessaries. These are devices usually made of silicone that get inserted into the vagina to help support the organs that have slipped out of place.
Treating uterine prolapse can greatly improve a patient’s quality of life. It’s important that doctors explain all available treatment options thoroughly, so patients can make informed decisions based on their needs and preferences.
Pelvic floor muscle training is typically taught under the guidance of a physiotherapist. These exercises have been shown to help ease a patient’s symptoms and improve certain medical scores that doctors use to assess how severe a condition is.
Results have shown that vaginal pessaries can be successful in treating uterine prolapse in a majority of cases. However, they don’t reverse the condition, instead they help to ease symptoms and slow down the progression of the prolapse. Patients usually need to try different types, sizes, and shapes of pessaries to find the one that fits them best.
It’s also important for pessaries to get checked regularly by a doctor to ensure they are not causing any irritation or infection. Rare complications can include the pessary moving into the bladder or rectum and causing a condition called fistula, which is an abnormal connection between organs.
Surgical treatment is another option for uterine prolapse, after taking into account factors such as a patient’s desire for future vaginal intercourse, personal and cultural beliefs about surgery, and awareness of potential complications. This can include a hysterectomy, a surgery to remove the uterus, which can be done either through the vagina or through the abdomen. There are also ways to preserve the uterus for those who would like to keep it for reasons such as fertility or personal preference. However, these patients will need regular follow-ups to monitor for any potential gynecological cancers.
A different surgical technique, called colpocleisis, involves stitching the vagina walls together to provide muscular support for the remaining pelvic organs. This is best for patients who don’t wish to have future vaginal intercourse.
What else can Uterine Prolapse be?
When a woman has symptoms suggesting a uterine prolapse, a doctor will usually confirm this diagnosis through a physical examination and a discussion about any related symptoms and medical history. However, they will also rule out other similar conditions that may present with comparable symptoms. These include:
- Urethral prolapse – a condition where the urethra (tube that carries urine) moves out of place and protrudes out of the body
- Cystocele – when the bladder sags down into the vagina
- Enterocele – when the small intestines drop down into the vagina
- Rectocele – when the rectum bulges into the vagina
- Abscess – a collection of pus that causes swelling in one area in your body
- Mass of gynecologic origin – swollen growth that is found in the female reproductive system
Ensuring an accurate diagnosis is crucial so that women can receive the most effective treatment.
What to expect with Uterine Prolapse
Uterine prolapse, while not a danger to life, can have significant effects on a person’s well-being. It can lead to feelings of low self-worth and anxiety, cause sadness or depression, and result in physical discomfort. It may also bring about problems with bowel and bladder control and impose restrictions on sexual activities.
Possible Complications When Diagnosed with Uterine Prolapse
When the muscles and tissues that hold the pelvic organs in place become weak, they can start to drop or slip out of place. This is called a prolapse. This weakness can affect the top of the vagina (the apical compartment), but it can also affect the front (anterior) and back (posterior) compartments. When these compartments prolapse, it can lead to further health problems, such as a cystocele (when the bladder drops into the vagina), a rectocele (when the rectum protrudes into the vagina) and/or an enterocele (when the small intestines push into the vagina).
These conditions often happen together and can cause urinary incontiness (leaking urine), fecal incontinence (loss of bowel control), and other long-term health problems.
Possible symptoms:
- Cystocele (bladder drops into the vagina)
- Rectocele (rectum protrudes into the vagina)
- Enterocele (small intestines push into the vagina)
- Urinary incontinence (leaking urine)
- Fecal incontinence (loss of bowel control)
Preventing Uterine Prolapse
When a doctor diagnoses a patient with a condition called uterine prolapse, it’s important for the patient to understand that this is a common and well-known health issue. The doctor will provide education about the possible outcomes and treatments, which can help the patient know what to expect and make them an active part of their own healthcare journey.
It can be easy for a patient to feel negatively about their condition, especially if they think it’s not “normal.” However, reassurance from their healthcare provider can help patients realize their condition is not unusual or unheard of. It’s a way to make them understand that uterine prolapse is not a cause for embarrassment or stigma.