What is Cervical Dislocation (Dislocated Neck Bone)?
Injuries to the neck, or the cervical spine, can be quite varied. They can range from muscle strain or damage to the membranes or ligaments surrounding the spine to displacements or dislocations of the spinal joints, sometimes along with fractures. Neck dislocations are significant and complicated injuries affecting the delicate vertebrae and the structures around the neck. They are commonly linked with traumatic injuries to the spinal cord. These injuries can press against the spinal cord and create serious neurological issues. How severe these injuries are depends on several factors. These include how strong the injury was, how much damage was done to the bones and soft tissues stabilizing the neck, the age of the patient, any existing syndromic conditions, the condition of the bones, and any other health conditions the patient might have.
A neck dislocation typically involves an unusual shift or misalignment of part of the neck. The neck or cervical spine is made up of seven bones or vertebrae. The C1 bone (also known as the atlas) connects with the base of the skull, while the C2 bone (also known as the axis) forms part of the main spine. The rest of the vertebrae, C3 through C7, are considered the lower part of the cervical spine. These bone structures are responsible for the movement and protection of the nervous system contained within.
The spine can be divided into three parts, each responsible for the stability of the neck. The front part includes the front longitudinal ligament and the front two-thirds of the vertebra and disc. The middle part includes the back longitudinal ligament, the back one-third of the vertebra and disc, and the back wall of the vertebra. The back part includes the pedicles, lamina, spinous process, and the posterior ligamentous complex. This complex, which includes the ligamentum flavum, facet joint or capsule, interspinous ligament, and supraspinous ligament, plays a key role in maintaining the stability of the spine. The stability of the neck and the treatment needed after an injury depend on how much damage has been done to its bones and the tissues that surround it.
What Causes Cervical Dislocation (Dislocated Neck Bone)?
Neck dislocations can happen at any age, and the cause of these injuries often depends on the age of the person involved. Neck dislocations typically result from traumatic events such as car crashes, falls, or sports accidents, usually leading to major impacts on movement and feeling.
Younger individuals often suffer neck dislocations due to high-speed accidents, like car crashes. In contrast, older individuals often experience neck dislocations due to less intense incidents, such as falling over at ground level.
A particular type of neck dislocation, facet joint dislocations, can either involve damage to the ligaments or include a broken bone. This kind of injury typically happens during a bending and pulling event and is commonly found in the lower part of the neck.
Movements with a lot of bending can produce a pull that causes the bones and ligaments at the back of the neck to give way under the strain. Meanwhile, a twisting or shearing force can result in a broken bone or even a dislocation.
Risk Factors and Frequency for Cervical Dislocation (Dislocated Neck Bone)
Cervical dislocations, or neck bone dislocations, can happen in two main places. The first one is the axial location, which includes the connection between the head and the first neck bone (occipitocervical), and the connection between the first and the second neck bones (atlantoaxial). The second one is the subaxial location, which involves the area starting from the connection between the second and third neck bones down to the connection between the seventh neck and the first chest bones.
While these dislocations can happen due to the instability of neck bones, which is often seen in children, most dislocations result from injuries like accidents. About 75% of such dislocations happen in the subaxial location, and men are the most affected group.
Kids under the age of eight are more at risk of suffering neck bone injuries. This is because their heads are larger in proportion to their body size, they have weaker neck muscles, and their ligaments are more flexible.
There are several red flags that can indicate the possibility of neck bone fractures in patients with multiple injuries. They include a fracture in the pelvic area, a fall or a head injury coupled with a pelvic fracture, high injury severity score (over 15), and being 40 years old or older.
- Cervical dislocations can take place in two main locations: axial (occipitocervical or atlantoaxial) and subaxial (C2/C3 to C7/T1).
- Involuntary neck bone movement can lead to these dislocations, especially in kids. But, most of them result from accidents.
- Most dislocations (about 75%) happen in the subaxial location, and they occur mostly in men.
- Kids aged 8 and under are at a higher risk of neck bone injuries due to their larger head, weaker neck muscles, and more flexible ligaments.
- Red flags that indicate possible neck fractures in patients with multiple injuries include: pelvic fracture, a fall or head injury plus pelvic fracture, high injury severity score, and being 40 or older.
Signs and Symptoms of Cervical Dislocation (Dislocated Neck Bone)
If someone suffers from a cervical spine injury due to a sudden, forceful impact, like in a car accident, it’s crucial to diagnose and manage it as soon as possible. Physical exams alone may not always correctly identify this type of injury, so understanding the individual’s accident details and conducting neurological tests, along with using imaging techniques, is vital. If there’s a suspected head or neck trauma, it’s crucial to immobilize the spine using a rigid neck brace to prevent further damage to the spinal cord.
During a trauma evaluation, the medical team needs to follow Advanced Trauma Life Support protocols. This process begins with assessing the patient’s airway and protecting the spine, then supporting the patient’s breathing and circulation, checking their neurological condition, and finally thoroughly examining the patient. After stabilization, a comprehensive examination can be conducted, which includes a detailed history, a physical exam, understanding the accident details, learning about any previous medical conditions that could lead to a higher risk of spinal injury, and looking for any other injuries.
Throughout the treatment process, regular neurological evaluations are necessary to monitor patient progress. Doctors usually use the American Spinal Injury Association spine exam to evaluate the patient’s neurological status, which focuses on important motor functions, sensory functions, rectal examination, and reflexes.
Patients who have had a cervical spine injury may show symptoms in their upper limbs due to nerve root injury or symptoms in both upper and lower limbs due to spinal cord injury. Before a complete ASIA exam can be performed, it’s important to determine if the patient is experiencing spinal shock, a temporary loss of spinal cord function and reflex activity. To evaluate this, the patient’s reflex response is checked by squeezing the penis or clitoris, or tugging on a catheter. If the patient does not respond, they are in spinal shock, which usually lasts from 24 to 72 hours. Accurate neurological examination can be performed when the patient is no longer in spinal shock.
Key Examination Findings:
- Occiput/C1: This is closely linked to the lower cranial nerves.
- Cranial nerves IX and X: They are tested through checking the gag response and observing any movement away from the affected side of the uvula.
- Cranial nerve XI: It is checked for its role in raising the shoulders and turning the head to both sides.
- Cranial nerve XII: It is tested for its role in sticking out the tongue and moving it side-to-side, while also looking for any small involuntary muscle contractions.
- C4: If this nerve root is injured, it can cause shoulder blade instability, leading to the shoulder blade sticking out because it majorly supplies the serratus anterior muscle.
- C5: If this nerve root is injured, it can lead to shoulder abduction and elbow flexion deficiencies (palm upwards), impacting the deltoid and biceps muscles. This could also cause sensory deficiencies in the outer arm and beneath the deltoid, along with an abnormal biceps reflex.
- C6: If this nerve root is injured, it can cause elbow flexion (thumbs up) and wrist extension deficiencies, primarily affecting the brachioradialis and the extensor carpi radialis longus muscles. There might also be sensory deficiencies in the thumb and the side of the hand, along with an abnormal brachioradialis reflex.
- C7: If this nerve root is injured, it can lead to elbow extension and wrist flexion deficiencies, majorly affecting the triceps and the flexor carpi radialis muscles. This could cause sensory deficiencies in the 2nd, 3rd, and 4th fingers, along with an abnormal triceps reflex.
- C8: If this nerve root is injured, it can lead to finger flexion, handgrip, and thumb extension deficiencies, primarily affecting the flexor digitorum superficialis, flexor digitorum profundus, and extensor pollicis longus muscles. This could also cause sensory deficiencies in the little finger.
- T1: If this nerve root is injured, it can cause finger abduction deficiencies, impacting the interossei muscles of the hand. This might also lead to sensory deficiencies in the inner part of the elbow.
Testing for Cervical Dislocation (Dislocated Neck Bone)
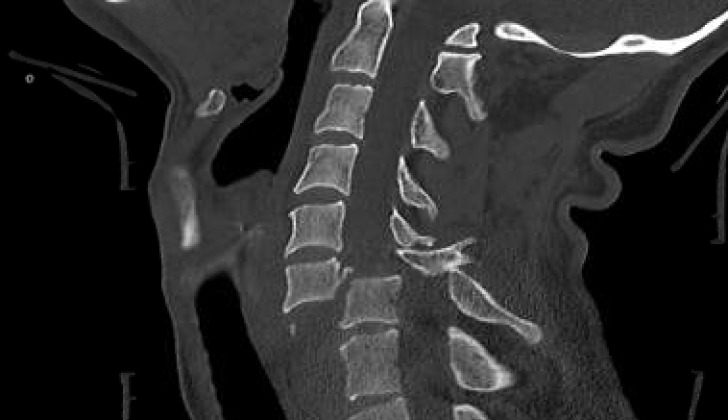
The usual process for creating images of the body in order to assess injury involves using X-rays, CT scans, and MRI scans. During an ordinary inspection for trauma, three different types of X-ray shots are taken – from the front (anteroposterior), from the side (lateral), and of the upper part of the spine through an open mouth (odontoid). These images should show the whole of the neck and particularly the area where the neck meets the upper spine (C7-T1 junction), as almost 1 in 5 spine injuries happen there. If this area isn’t clearly shown on the usual three shots, another one, known as a swimmer’s view, can be taken to check the spine’s alignment from the side.
Signs of damage to the joints between the spine bones can include a bone moving out of its usual position compared to the one below it. This can be seen if there is a change or disappearance of the usual curve of the neck when looking at four lines that should be parallel along the spine. Damage to one side of the spine joint can lead to a about quarter of the bone moving out of place, while damage to both sides can result in about half of it moving out of place. If the spaces between the bones seem smaller, this could mean a spinal disc has been pushed back towards the spinal canal. CT scans are increasingly being used first to evaluate trauma because they are better at showing the shape of the bones than X-rays, particularly around the C7/T1 area.
There are some specific features that can be seen on a CT scan to show instability or displacement of the neck bones. These include the following.
The area where the spine meets the skull can be assessed for displacement using the “power ratio”. This is a calculation comparing measurements, with a result of 1 being normal, more than 1 indicating forward displacement, and less than 1 indicating backward displacement. Another measurement often used is the distance from the basion (a part of the skull) to the tip of the dens (a part of the second neck bone); if this is over 12 mm it can suggest a separation between the head and the neck.
The lower part of the neck can also be assessed. Displacements of the joints between the bones are usually easiest to see from the side. One should look at the CT scan from the side to check the positioning of the front and back parts of the bones and the lines along the back of the spine; these should all be smooth and continuous. Looking from the top or bottom, the joint surfaces should be flat, appearing as a hamburger, with the meat in between the buns. Any signs of displaced bones or joints could indicate instability.
The so-called ‘naked facet sign’, also known as the ‘hamburger’ or ‘reverse hamburger bun sign’, seen when looking down on the spine, shows up when a joint has dislodged. This is a signal of instability in the spine, with the burger pieces representing the joint, and the meat in the middle representing the space created in between the dislodged joint.
MRI scans are very good at showing disc herniations (displacements) and any injuries to the spinal cord, nerve roots, and the ligaments at the back. However, they are not as effective as CT scans in showing the shapes of the bones. They are, therefore, recommended only for those with abnormal neurological examinations, or in unconscious or intoxicated patients who are suspected of having a spinal cord injury.
Treatment Options for Cervical Dislocation (Dislocated Neck Bone)
The first key step in handling neck injuries, known as cervical trauma, involves accurately distinguishing the type and severity of the injury. This allows physicians to decide on the best course of action, which could be either surgical (involving an operation) or nonsurgical treatment.
Timing
One might assume that rapid treatment would improve outcomes for spinal trauma. Yet, some studies reveal no big difference in results for patients who underwent early surgery compared to those receiving the procedure later on. As such, going into surgery within the first 72 hours after trauma, depending on the patient’s health and additional conditions, seems to be an acceptable option.
Conservative Treatment
A cervical brace is used mostly for neck fractures that do not involve significant shifting, dislocation, or excessive curvature. These fractures often occur from trauma and usually need some type of stabilization surgery.
In the past, high-dose steroids were used within the first 8 hours after a spinal cord injury. But recent studies suggest that this increases the risk of lung infections and bleeding in the stomach. Today, steroids are still used, but at much lower dosages.
In most cases, physicians opt for surgical treatment when there are neck joint dislocations. These typically injury the spinal cord and require support to stabilize the spine. Depending on the number of injured parts, the treatment may range from managing single to multiple spinal levels.
Operative Treatments
There are various surgical procedures, and the right choice depends on the patient’s situation and injury severity.
For patients presenting with unilateral or bilateral facet dislocation and neurological deficits, a procedure involving immediate closed reduction followed by MRI and surgical stabilization is typically used. In the process, devices are attached to the patient’s head to apply incremental weight, which aids in relocating the dislocation. Medical professionals monitor the patient closely, with frequent neurological exams and x-rays.
For cases where patients do not respond well to closed reduction or have certain other conditions, immediate MRI followed by open reduction and surgical stabilization is used.
In situations where a significant anterior spinal cord compression is detected after an MRI, the surgery involves anterior open reduction and anterior cervical decompression and fusion. This surgery is less effective for bilateral facet dislocations.
If a reduction cannot be achieved with closed or anterior techniques, posterior reduction and instrumented stabilization is implemented. New developments in neuronavigation have led medical professionals to preference pedicle screws over lateral mass screws due to the improved stability.
In some situations, a combination of two methods is needed, starting with anterior decompression followed by a posterior strategy.
Management of Associated Conditions
Due to a high risk of deep venous thrombosis, patients receive compression devices immediately, and if considered safe, get chemical prophylaxis within 72 hours. Proper steps ensure that hypotension is avoided and sinus bradycardia, the most common rhythm problem after a spinal cord injury, is managed.
Relieving pain and managing symptoms associated with abnormal autonomic responses are also key. Bladder and bowel care, crucial aspects of treating acute spinal cord injuries, aim to preserve upper urinary tract structures and lower incidences of urinary tract infections.
Mobilization
Physiotherapy and occupational therapies ideally start within the first week after the acute spinal cord injury. These begin once the patient’s condition becomes stable, even if they require sedation, vasoactive support, or mechanical ventilation.
What else can Cervical Dislocation (Dislocated Neck Bone) be?
When doctors are dealing with neck dislocations, they have to think about a variety of possible spinal injuries. This careful approach helps determine the exact problem and the best approach for treatment. Conditions that can mimic neck dislocations include:
- Blunt trauma to the neck
- Different types of neck fractures (such as Jefferson, Hangman, Burst)
- Damage to certain parts of the spine (spinous and transverse processes)
- Neck strain injuries
- Penetrating injuries to the neck
- Blockage or damage to the spinal cord’s blood supply
- Shock due to low blood volume
It’s important for the doctor to thoroughly analyze these possibilities to ensure an accurate diagnosis and the best possible treatment.
What to expect with Cervical Dislocation (Dislocated Neck Bone)
Complete spinal cord injuries often improve by different degrees in most patients. Roughly 80% of patients improve by 1 ASIA grade, a measure for assessing the severity of the spinal cord injury, while about 20% of patients improve by 2 grades. Complete recovery, however, only happens in about 1% of patients at the time of hospital diagnosis. Two primary factors that affect the prognosis are the patient’s initial neurological condition and the time it takes to perform the surgical decompression and stabilization.
Here are some examples of how the level of spinal cord injuries can affect daily function:
* C1 to C4 injuries: Patients typically depend on a ventilator for breathing and rely on an electric wheelchair, which is controlled by movements of the head and chin.
* C5 injury: Patients can breathe without a ventilator and have muscle function in the biceps and deltoids, allowing them to bend their elbow. However, they cannot rotate or extend the wrist, meaning they are unable to feed themselves. These patients operate an electric wheelchair with hand control and can carry out daily life activities independently.
* C6/C7 injuries: Patients have the ability to bring their hand to their mouth owing to an intact wrist extension and rotation. This makes it possible for them to feed themselves. These patients live independently, use a manual wheelchair, and can even drive using manual controls.
* C8/T1 injuries: Patients have better hand and finger strength and dexterity, which allows them to transfer independently.
Possible Complications When Diagnosed with Cervical Dislocation (Dislocated Neck Bone)
Cervical dislocations, whether they are treated with surgery or not, can result in serious and complex health issues.
After undergoing a surgical procedure, patients can experience a range of complications such as:
- Infection
- Injury to the vertebral artery and carotid artery
- Difficulty swallowing (dysphagia)
- Damage to the recurrent laryngeal, superior laryngeal, and hypoglossal nerves
- Horner syndrome (a condition affecting the face and eyes)
- Creation of a false joint (pseudoarthrosis)
- Disease in the segments above or below the treated one (adjacent segment disease)
Other problems include:
- Skin problems: These usually occur in persons who are paralyzed in all four limbs (tetraplegic or quadriplegic). Prevention and good skincare are essential, along with frequently changing the patient’s position.
- Major depressive disorder: After a spinal cord injury, it’s not uncommon for patients to experience depression, sometimes severe enough to cause thoughts of suicide. It’s essential to educate patients about this risk and to treat any signs of depression promptly.
- Blood clots (venous thromboembolism): This issue arises from blood pooling and clotting in the veins. Using blood thinners right away, applying pressure to the legs, and getting up and moving around as soon as possible can reduce this risk.
- Urosepsis: Patients who lose control over their bladder can develop a serious bloodstream infection due to bacteria in the urine. It’s crucial to use clean techniques when catheterizing these patients and prevent overfilling of the bladder, as this can increase the risk of urinary tract infections.
Recovery from Cervical Dislocation (Dislocated Neck Bone)
After surgery for neck dislocations, attentive post-operative care and rehabilitation are vital to support a patient’s recovery and improve their ability to function. Directly following the operation to fix the neck, patients require careful watching. This is to check for changes in their nervous system function, manage pain, and minimize the chance of complications like infections or issues with surgical implants.
Next, the focus is on rehabilitation, which aims to bring back mobility and strength, as well as enhance awareness of body position and movement. This includes a personalized program of physical therapy, occupational therapy, and therapeutic exercises. The patient’s activity levels are slowly increased, paying attention to maintain correct body alignment and stable spine.
It’s also necessary to educate patients about correct body movement, workplace ergonomics and ways to prevent injuries, for lasting spine health and to lower the chance of reinjury. Finally, ensuring open communication and collaboration among all healthcare professionals – including surgeons, therapists, and primary care doctors – is key to providing holistic care and helping patients reach their functional goals.
Preventing Cervical Dislocation (Dislocated Neck Bone)
Talking to patients and teaching them about spine health is very important for preventing neck injuries like cervical dislocations. People should know how they can injure their necks, like by not wearing a seatbelt or not using safety equipment during sports. It’s also important to avoid any actions that could lead to slips or knocks. Learning how to lift things properly, keeping a good posture, and understanding workplace ergonomics can also help protect the neck.
Being able to recognize the signs and symptoms of a displaced neck, and understanding the importance of swift medical care if neck injury is suspected, is crucial. By giving patients this information and practical advice, healthcare professionals can help lower the likelihood of these injuries, and keep our spines healthy.
If someone has suffered from a cervical dislocation, their doctor might suggest they see a physical therapist. This expert will come up with a recovery plan that suits the patient’s specific needs. They’ll recommend the best ways to ease pain and improve neck movement, and give advice on how to take care of their neck to avoid further harm.
The patient’s own actions towards recovery are just as important. Some things they can do at home include using ice and heat to soothe pain, doing neck exercises, and training to improve their posture. These steps ease the pressure on the troubled area and significantly lower the chances of a repeat injury.