What is Humeral Shaft Fractures?
The humerus, which is the single long bone in the upper arm, can sometimes break or fracture. These fractures represent 1-5% of all types of bone fractures. The age groups most likely to experience this type of fracture are young people, often due to severe injuries, and older individuals who experience it due to less powerful forces.
The humerus connects to the shoulder blade at the top and to the forearm bones at the bottom. The upper part of the humerus has a head, neck, and two bumps called tubercles, with the humerus head forming a joint with the shoulder blade. Below these tubercles is a narrow section known as the surgical neck, which is a frequent location for these fractures.
On the side of the humerus is a bump where a muscle called the deltoid attaches. In the middle of the humerus, there’s a small dip, known as the radial groove, where a nerve and an artery pass through. This area is susceptible to injury if there’s a middle-third fracture of the humerus. The lower part of the humerus widens and forms projections.
The arm is divided into two sections. The front section contains the main nerve and blood supply to the arm, along with several muscles and three main nerves. The back section contains the muscles of the triceps and another main nerve.
In the past, most humerus fractures were treated without surgery, especially with the invention of a special brace. However, some fractures of the humerus now require early surgery for better recovery.
What Causes Humeral Shaft Fractures?
The bone in your upper arm, called the humerus, can break in different ways – either from a hard hit or a gentle impact. High-force impacts can happen from a solid punch to the arm. Most commonly this might happen from things like car accidents, sports activities, accidents at work, or a physical attack.
On the other hand, fractures from low-impact, or gentler causes, typically occur from indirect trauma like falling on your hand when your arm is stretched out. In this case, the force from the fall gets passed up the arm to the humerus. This type of injury is more common in older people or individuals with bone diseases.
Knowing how the break happened is essential in identifying the type of fracture and next steps in care. This can be a useful clue in spotting any other injuries that may have occurred at the same time.
Risk Factors and Frequency for Humeral Shaft Fractures
Humeral shaft fractures, which are breaks in the upper arm bone, make up 1-5% of all fractures. These fractures are most likely to occur in two age groups: those in their 30s and those in their 70s. Younger patients generally experience these fractures due to high-impact injuries, while older patients are more likely to have low-impact injuries.
About 60% of humeral shaft fractures happen to patients over 50 years old. Interestingly, among those under 50 with this type of fracture, about 70% are men. On the flip side, approximately 70% of patients over 50 years old with humeral shaft fractures are women.
Lastly, the most common spot on the upper arm bone to fracture is the middle section, making up around 60% of all humeral shaft fractures.
Signs and Symptoms of Humeral Shaft Fractures
If you have a humeral shaft fracture, the primary symptom you’ll notice is pain in your upper arm where the injury has occurred. Your doctor will want to know exactly how the injury happened. Severe injuries usually go along with other types of damage, so a full-fledged trauma team may be needed to check you from head to toe. On the other hand, if your arm was injured through a minor accident, your doctor might suspect that a disease such as osteoporosis caused a pathologic fracture – that’s when a bone breaks in an area where it was already weak.
During the physical examination, the doctor might see that your upper arm is misshapen, swollen, or bruised. If your fracture is below the deltoid muscle – that’s the big shoulder muscle – your arm could be angled inward. The doctor will carefully inspect your skin to see if the fracture has broken through, resulting in what’s called an open fracture. Sometimes, the skin might be pushed upward from the inside by the broken bone pieces, which suggests an open fracture might happen soon. The doctor will also check places that might be overlooked, like your armpit and the back of your arm.
Then it’s time for the neurovascular exam. In plain English, that’s when the doctor checks if your nerves and blood vessels are working properly. This is done methodically, from the shoulder towards the hand. One important thing your doctor will look for is a condition called radial nerve palsy. This occurs in 2-17% of people with humeral shaft fractures, and it causes weakness in your wrist and finger extensors – the muscles that help you open your hand and straighten your fingers.
The doctor will also check your brachial artery. This check can be done by examining your distal radial and ulnar pulses – that’s the pulses on the thumb side and pinky side of your wrist – and seeing how quickly your fingernails regain their color after being pressed. If your blood flow or nerve function seem different after any initial treatment, your doctor may order more imaging tests and consider surgery to correct the issue.
Testing for Humeral Shaft Fractures
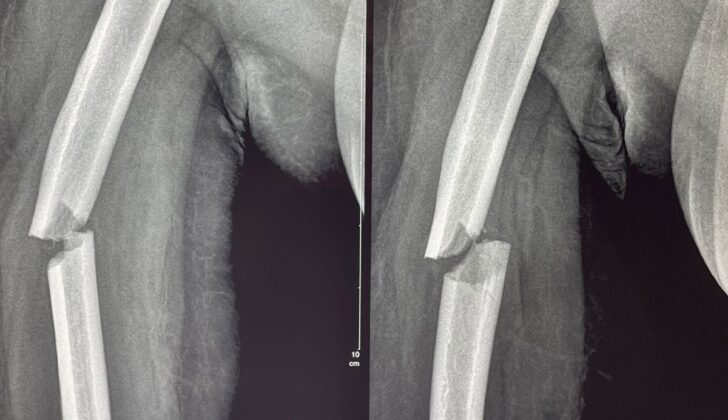
If your doctor suspects that you have a fractured humerus (the long bone in your arm), you will need to undergo several tests. Initially, they will perform an exam to check your blood vessels and nerves. You will also need x-rays of your humerus, which includes the shoulder and elbow joints, taken from at least two different angles. This will help the doctor understand more about your injury.
If you’ve had any recent meals, are using blood thinners, or have other health conditions, it’s important to let your doctor know, as these factors may influence the decision to perform surgery right away. If there is any suspicion of blood vessel injury, you might need a special type of CT scan known as computed tomography angiography (CTA). If the injury has affected the function of your radial nerve, this should be documented before any attempts are made to reset the bone.
The x-rays of your humerus allow doctors to study the type and extent of your injury. The humerus itself is divided into three segments for easier identification – the top, middle, and bottom. The fracture type could be transverse, oblique, spiral, edge, or comminuted (shattered), and this will dictate the surgical approach if one is needed.
Decisions about treatment will mainly depend on information obtained from your x-rays. Some cases which would call for immediate surgery include open fractures, fractures that need vascular repair, a ‘floating elbow’ fracture resulting from an arm bone fracture on the same side, nerve injuries, complications like compartment syndrome and fractures near prosthetic joints. Other factors, such as the complexity of the fracture, significant tissue damage and whether multiple limbs are involved, will also be considered in the decision-making process. If your injury is closed (without broken skin) and isolated, with no immediate risks, your doctor might choose to temporarily immobilize it and re-evaluate it later on an outpatient basis.
Treatment Options for Humeral Shaft Fractures
Arm injuries can often be treated without surgery. For example, closed fractures, where the bone fragments are not exposed through the skin, can be treated through a process called ‘closed reduction’. This involves applying pressure and other forces to correct the abnormal shape of the bone. Afterward, a splint or cast is used to keep the bone stable. This process usually requires more than one healthcare provider.
When it comes to fractures of the humerus (upper arm bone), doctors tolerate some certain degrees of deviation from the correct bone shape. These deviations are typically enough to maintain the long-term function of the arm without needing surgery.
After the initial immobilization, the patient’s splint or cast may be changed to a different type of brace 7 to 10 days later. This helps keep the bone aligned and allows for recovery. In fact, about 94% of closed fractures that are managed this way heal well. Once healed, patients can start weight-bearing exercises to strengthen the arm, and a physical therapist can help them regain full function.
However, not all arm injuries can be treated conservatively. Open fractures, where the skin is broken and the bone is exposed, require more intensive interventions, including intravenous antibiotics to prevent infection and possible early surgery for large soft tissue injuries. Other injuries that often require surgery are those associated with damage to the blood vessels or nerves, fractures of the upper and lower arm on the same side (known as ‘floating elbow’), or compartment syndrome, which is a dangerous buildup of pressure within the muscles.
Surgical treatment of the humerus can be performed in several ways, including external fixation where pins are placed outside the skin to hold the reduced fracture, and open reduction and internal fixation (ORIF), where the bone fragments are manipulated directly and fixed in place using plates and screws. The surgical approach is chosen based on the patient’s condition and the location and pattern of the fracture. The healing process after surgery will depend on the type of fracture. With simple fractures, the bone fragments can connect directly, while more complicated fractures will go through several stages of healing.
In conclusion, while non-surgical treatment of humerus fractures can be successful, recent studies have shown that surgical intervention can promote faster recovery, especially for patients with multiple injuries.
What else can Humeral Shaft Fractures be?
Fractures in the humerus, or upper arm bone, can be grouped according to where they are located and how severe they are. These fractures can happen at different points of the humerus – near the shoulder (proximal), the middle, or near the elbow (distal) – and each location can be associated with different types of injuries. Knowing the exact location of the fracture is crucial for effective treatment.
There are also other conditions that cause pain in the arm such as dislocated shoulders and elbows, tears in the tendons and muscles, nerve-related conditions (neuropathies), and inflammation of the soft tissues due to things like infections and bruises. However, these conditions each affect different areas and have different causes, and they come with their own unique set of symptoms.
What to expect with Humeral Shaft Fractures
Humeral shaft fractures, or breaks in the long bone of the upper arm, typically have a positive outcome. When these fractures are treated non-surgically, the rate of them not healing properly ranges from 3% to 17.6%. On the other hand, fractures treated with surgery generally heal well, but this approach can also lead to high surgical expenses and potential complications with the soft tissues surrounding the fracture after the operation.
Patients might need to keep their arm immobilized for up to 10 weeks after the injury. Physical therapy can be beneficial in helping patients get back their full strength and movement in the arm.
Possible Complications When Diagnosed with Humeral Shaft Fractures
Humeral shaft fractures, or breaks in the long bone in the upper arm, can lead to various complications. There are complications related to either nonoperative or surgical treatments. Nonoperative complications may include skin irritation from the cast or splint, or the fracture getting worse. On the other hand, surgical interventions may lead to complications such as infections, wounds not healing, the failure or prominence of medical devices implanted during surgery, and severe pain often experienced after intramedullary nailing, a type of surgery where a metal rod is inserted into the marrow canal of the bone.
Non-union and radial nerve palsy are complications that could occur because of or independent of the treatment process. Non-union refers to a bone not healing 6-12 months after an injury. ‘Delayed union’ refers to when the bone takes 4-6 months to heal. An important indicator of nonunion is the absence of new bone formation (callus), and continuous movement at the fracture site 6 weeks post-injury.
Two types of non-union occur due to different reasons. ‘Atrophic nonunion’ happens when the bone fails to heal due to problems with the bone healing process or the body’s inability to repair bones. Common causes can be infections, lack of certain vitamins, arterial diseases, weakened immune system, and disease affecting connective tissues. It is essential to identify the exact problem through diagnosis and patient history review to take corrective measures. It is also important to inform the patient about lifestyle changes, such as quitting smoking and controlling blood sugar levels.
The second type known as ‘hypertrophic nonunion’ usually happens due to instability at the fracture site, and it is identified by excessive new bone (callus) formation without connection at the fracture site on an X-ray. This type often requires surgery to stabilize the fracture and promote healing.
Radial nerve palsy often accompanies these fractures – particularly spiral fractures in the lower section of the upper arm bone. This condition affects about 11.8% of humeral shaft fracture patients. Surgery isn’t always necessary as most cases (70-90%) recover naturally within 2-3 months. However, if immediate surgery is required in emergencies, this condition needs to be addressed. A ‘cock-up’ wrist brace can assist in managing wrist drop and preventing muscle shortening, or ‘contractures’. The function in this nerve usually returns, starting with the brachioradialis muscle, which helps extend and move the wrist sideways. Restoration of function in the index finger extensor muscle is generally the last to occur.
If the patient shows no improvement after 2-3 months, a nerve conduction study or electromyography (EMG), a test to evaluate the electrical activity produced by muscles, is recommended. If abnormal muscle activity is detected during this test, or if the patient still doesn’t show any improvement after 4-6 months, surgery is usually the next step. If the function of the radial nerve does not improve after surgery, a tendon transfer surgery might be needed to restore as much wrist and finger extension as possible.
Recovery from Humeral Shaft Fractures
After an injury or surgery, patients usually have a period of time where they don’t move too much. Over the next six weeks to three months, they should be able to move more and start to bear more weight. At the start, patients use their other arm or a physical therapist helps them to move their elbow and shoulder. As they get better, they can begin to work on moving their arm by themselves and start to bear weight.
Preventing Humeral Shaft Fractures
When dealing with a humeral shaft fracture, or a break in the long bone of the upper arm, it’s important for patients to understand the nature of their injury, their treatment options, and the rehabilitation process. This means breaking down all the complex medical terms into simple language. We should also share findings from any physical exams or imaging tests done.
We can discuss the treatment options but let’s remind patients that treatments are personalized. Depending on their particular situation, a non-invasive treatment or surgery might be the best option. It’s crucial to explain the pros and cons of each option.
Once we’ve decided on a treatment plan, we need to explain what they should expect during the process. If we’re taking a non-invasive approach, patients need to know how to manage pain, when to use ice, how to position their arm, and which other medications they might need to take at home. It’s also important to include information about warning signs of serious problems that need immediate medical attention. We should provide a schedule of follow-up appointments and any necessary tests. If surgery is the chosen approach, we need to share the schedule and provide instructions for preparation.
We should also talk about risk factors for these fractures to help patients understand and prevent future breaks. If certain medical conditions or behaviors increase the risk, we’ll discuss them with the patients and suggest any necessary lifestyle changes.
During recovery, patients need to know how long healing typically takes and what activities to avoid. It’s important to highlight that physical therapy will play a big role in recovery. If the injury has caused emotional distress, we should provide support, reassurance, and consider referring them for counseling or psychological therapy.
In the end, the goal of patient education is to meet the individual needs of each patient. By actively involving patients in their healthcare decisions, we can empower them to participate actively in their recovery.