What is Lumbosacral Disc Injuries?
The space between the lower back (lumbar) and the tailbone (sacral) is more prone to injuries due to the change in movement dynamics in these areas. Between each back bone (vertebral body), there exists a cushion-like structure called the intervertebral disc. This disc is made of a tough outer layer (annulus fibrosus) and a softer inner layer (nucleus pulposus). It works to provide support and flexibility while also carrying minor load.
Damage to the annulus fibrosus might lead to wear and tear or a bulging of the inner nucleus pulposus. This bulging can press on the spinal cord or nerve root, which can result in pain and weakness.
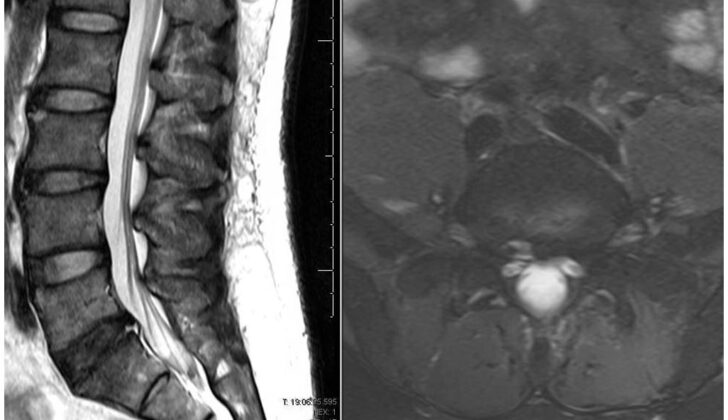
More than 90% of herniated discs, which are bulging discs, occur in the L4-L5 or the L5-S1 disc spaces, referring to specific areas in the lower back. If the disc injury becomes severe enough to cause nerve damage or interfere with daily activities, surgery could be needed to relieve pressure and stabilize the affected segments. However, before resorting to surgery, non-surgical treatments like pain relievers, changing activities, and injections are typically tried for several months, especially if there are no signs of weakened muscles.
What Causes Lumbosacral Disc Injuries?
Contrary to popular belief, there’s no solid evidence that repeated bending forward actions are directly linked to disc injury. Previously, jobs involving heavy lifting were thought to be associated with a higher risk of this type of injury to the discs in your back, also known as intervertebral disc disease. However, now it is believed that these connections might be influenced by other factors. These factors could include a lower socioeconomic status or certain lifestyle habits of individuals in these jobs.
Fascinatingly, recent studies have revealed that our genes play a significant role in disc injuries and spine degeneration, that is, wearing down of our spine over time. This was backed by research involving identical twins (scientifically known as monozygotic twins). An example of one study looked at MRI scans of 115 identical twins. The results showed that genetics accounted for about 34% of the differences in disc degeneration of the lower spine (versus only 2% for physical load and 7% for age). This suggested a notable genetic component to these conditions.
Risk Factors and Frequency for Lumbosacral Disc Injuries
The understanding and frequency of disc injuries have evolved due to advancements like MRI technology. Determining the exact rate of disc degenerations can be challenging as many of these cases often have no symptoms. To make matters more complicated, there isn’t a uniform definition for disc degenerations and disc herniations, making it hard to compare the disease’s prevalence across various studies.
In a review of 20 studies using MRI on individuals without symptoms, the reported instances of disc abnormalities varied. Here’s a breakdown:
- 20% to 83% showed reduced signal intensity
- 10% to 81% had disc bulges
- 3% to 63% had disc protrusions compared with 0% to 24% for disc extrusions
- 3% to 56% had disc narrowing
- 6% to 56% were found with annular tears
This study indicates that finding disc disease unexpectedly is not unusual and doesn’t necessarily call for specialist evaluation unless there is pain or limitations.
Signs and Symptoms of Lumbosacral Disc Injuries
When a patient has back pain, doctors need to learn more about the start of the pain, if there is any radiating pain (pain that spreads to other parts), and if there were any injuries or accidents that might have caused it. They should also check for several aspects including:
- Changes in back pain or symptoms based on different postures (like bending forward or lying down)
- The patient’s ability to walk without any symptoms
- Previous symptoms, injuries or surgeries
- Weakness, tingling or numbness
- Signs of illnesses, unexplained weight loss, or recent travel
Back pain that spreads, or “radiates”, often has more predictable surgical outcomes compared to general lower back pain. This general lower back pain could be due to tired or strained muscles. Back pain that is linked with certain movements might mean there’s instability or a degenerative fracture at L5, a specific area of your spine.
To understand how the pain affects the patient’s daily life, the doctor needs to observe the patient’s way of walking. The doctor might ask the patient to get up from a chair, walk on their heels and toes, and then climb onto the examination table. This allows the doctor to test strength, reflexes, and perform a straight leg test. A complete exam involves checking the neurological function of the arms, legs, bladder, and bowels. It’s necessary to be thorough and patient during the exam. Doctors also need to search for any feelings of tenderness along the patient’s back, any previous surgical scars, and check the sensation and reflexes.
The straight leg test involves having the patient lie flat and stretch their leg from 0 to about 80. If this causes radiating back pain in either leg, it could indicate a diagnosis of a stenotic canal, a narrowing of the spinal canal.
Disc herniations at the L5/S1 level, a specific area of your spine, can have two main presentations:
- L5 disc herniation- if the herniated disc at L5/S1 level goes far into the left or right neural foramen (a gap between two vertebrae), it may compress the L5 nerve. This could lead to weakness of the hip abduction muscles, ankle dorsiflexion (muscle in front of your ankle), or extension of the big toe.
- S1 disc herniation- if the herniated disc at L5/S1 level goes centrally into the canal, it may compress the S1 nerve. This could lead to weakness of the ankle’s plantarflexion (back muscle of ankle).
Testing for Lumbosacral Disc Injuries
If you’re suspected of having an injury to the lumbosacral disc (which is a part of your lower back), certain clinical tests can help with the diagnosis. According to a 2011 study, people with a positive result on two tests, called the straight leg test and Achilles reflex test, are likely (79% chance) to have an issue where the nerve roots in the low back are squeezed or pinched (known as nerve root impingement). If you have a positive straight leg test on both legs, it further increases the certainty (from 84% to 96%) that you have a lower back disc herniation.
Your doctor may also want to get a front-to-back and side view X-ray of the part of your spine that is causing problems. If there are strong warning signs (or “red-flags”) of a serious problem with your lumbosacral disc, your doctor may order a magnetic resonance imaging (MRI) scan to get a more detailed image which could be used to plan possible surgery. These red flags could include cauda equina syndrome, which is a serious issue where you may not be able to control your bowel or bladder, difficulty urinating, a suspected infection (especially if you’re prone to infections e.g., due to drug use), nighttime chills or a history of fever. Other red flags could be a suspected tumor (especially if you’ve had cancer before or are losing weight unexpectedly) and trauma (like a fall, assault, or collision).
It’s important to point out, though, that if you have typical symptoms of a lower back muscle strain, you might not need an X-ray or any other type of imaging. However, if the symptoms don’t get better or you have worrying results from a physical examination, the doctor may then recommend an X-ray. They might also consider additional X-rays that show your back while you’re bending and straightening, especially if they think you might have movement or slippage (spondylolisthesis) of a vertebrae. Normally, in these situations, an MRI isn’t needed right away unless those red flags we talked about earlier are there. Doctors typically recommend a six-week course of physical therapy first. If, after physical therapy, you’re still experiencing symptoms, they might then suggest an MRI.
One interesting observation is that, over time, disc herniations (or a type of injury to the disc) will appear smaller on an MRI, whether they cause symptoms or not. Also, finding disc disease (like wear and tear or disc herniation) on an MRI does not mean you are more likely to have long-term pain or a future need for surgery.
Treatment Options for Lumbosacral Disc Injuries
Good news is that more than 90% of people with L5/S1 disc injuries (the disc located between the last lumbar bone and first sacrum bone of the spine) tend to improve without the need for surgery. A non-surgical approach generally includes six weeks of physical therapy, which primarily focuses on strengthening the core muscles and performing stretches.
Other non-surgical strategies involve changing activities that might worsen the pain, taking anti-inflammatory medications, and having epidural injections. Epidural injections, which are injections given into the back to reduce pain and inflammation, may offer moderate and temporary relief for lower back pain caused by disc herniations. However, the effectiveness of these injections for ongoing back pain that doesn’t radiate to other body parts is less certain. In some instances, injections may be targeted to the facet of the L5/S1 if MRI scans show this area has increased inflammation.
If these non-surgical strategies don’t provide enough relief, the patient is usually left with three options- continue to live with the pain, avoid activities that cause pain, or consider surgical intervention. According to a study published in the Spine Patient Outcomes Research Trial (SPORT), patients who chose surgery typically had better outcomes after three months, two years, and four years compared to those who didn’t have surgery.
There’s ongoing research about the best surgical method, surgical approach, and when to use decompression or instrumentation devices. Based on what we know currently, traditional open surgery and microdiscectomy (a less invasive procedure that involves removing parts of a herniated disc) are both effective. If a surgical procedure called a discectomy is chosen, removing a small amount of the disc (limited discectomy) provides better pain relief and patient satisfaction than removing most of the disc (subtotal discectomy), but there is a higher chance of the herniation happening again.
Interestingly, patient satisfaction and outcomes seem to be the same whether it’s their first or a repeated microdiscectomy. The operation may require staying in the hospital overnight, but most times it’s intended to be a day procedure. It’s important for patients to understand that while surgery often provides favorable results in relieving radiating pain (pain that extends to other areas), the outcomes for non-radiating lower back pain can be less predictable.
What else can Lumbosacral Disc Injuries be?
Here are some potential causes of abdominal pain in elderly people:
- Acute aortic dissection (a tear in the large blood vessel branching off the heart)
- Cauda equina (a bundle of spinal nerve roots)
- Constipation
- Epidural infections (infections in the spinal cord)
- Herpes zoster (shingles)
- Mechanical back pain (pain resulting from physical strain)
- Nephrolithiasis (kidney stones)
- Osteomyelitis (bone infection)
- Sickle cell anemia (a group of blood disorders)