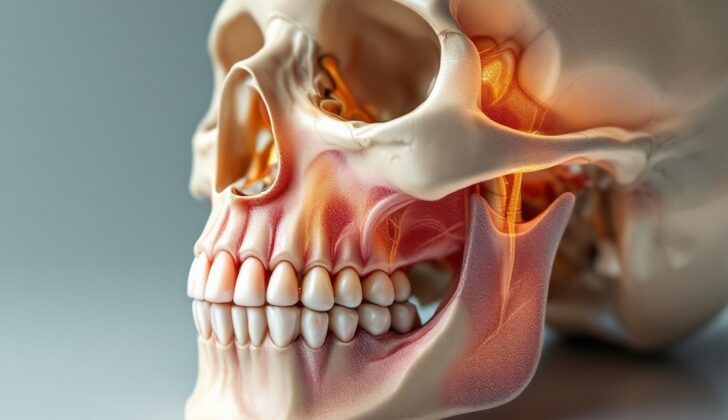
What is Maxillary Fracture?
Fractures to the upper jaw, or ‘maxillary fractures’, are quite common in emergency situations. Because the upper jaw is closely linked to important structures in the body, including the brain, it’s really important to correctly diagnose and plan the right treatment quickly. There are many different treatment methods used all over the world, and their main goal is to get the patient’s quality of life back on track.
What Causes Maxillary Fracture?
What causes fractures in the upper jaw varies from place to place. It depends on the country’s economic status, popular sports, car rules, and other laws.
In adults, upper jaw fractures usually happen because of high-risk activities like fighting or car accidents. Motorcycle accidents are the most common causes of these injuries, followed by regular car accidents. A large fraction of these incidents involve alcohol or illegal drugs. Another common cause is violence – about 19% of upper jaw fractures in a Swiss research study were due to fights.
Sports injuries also account for a significant number of upper jaw fractures – between 6% and 33% of them. The cause often depends on which sports are popular in the country. For instance, the Gaelic football, soccer, rugby, and horse riding are the main sports linked to upper jaw injuries in Ireland, while soccer is the main cause in Italy, Germany, and France. In counties like Switzerland and Austria where skiing is popular, it’s the most common sport causing injuries.
For children and older people, the main cause of upper jaw fractures is falls. Serious fractures are rare in kids and usually occur in major accidents, like car crashes. In older people, these injuries are often associated with other severe health problems, increased severity of the fracture, and a higher risk of dying.
Risk Factors and Frequency for Maxillary Fracture
A study from Malaysia found that injuries to the upper jawbone (maxillary) are quite common in males, making up 82.2% of the cases in a pool of 473 patients. The average age of these patients was around 30 years old, with the oldest being 87 and the youngest just seven months. These injuries were most frequent in people aged 11 to 20 (34.5% of cases) and then 21 to 30 years old (23.3% of cases). This trend could be due to the increased likelihood of engaging in high-risk activities, sports, and encountering violence among these age groups. These findings were echoed in a study from Royal Perth Hospital in Western Australia where males made up 87% of cases and the average age was 27. As people get older, however, the trend towards male dominance decreases, perhaps because falls become the leading cause of fractures in general.
- In people under 18, fractures become more likely as they get older, possibly due to more engagement in high-risk activities and changes in the body’s physical structure.
- Gender dominance is not observed in young age groups, but it becomes apparent during late childhood and teen years.
- Facial fractures are unusual in children under 5, as they represent only 1.4% of cases.
Signs and Symptoms of Maxillary Fracture
If someone is suspected to have a broken upper jaw, or maxillary fracture, they need to be quickly examined because there could be other dangerous injuries. Professionals first have to do an overall check, which includes a complete trauma assessment. Help from an emergency medical team may be needed at this point. Once the person is stable, the medical team needs a detailed account of what caused the injury. It’s crucial to know if the person passed out or shows signs of a head injury because they might need urgent neurological care. The medical team also has to know when the person last ate and what medicines they take in case they need surgery.
The person also needs a more detailed check for other injuries. This includes:
- Checking over the outside of their mouth for pain, swelling, bleeding, bruises, and nosebleed.
- Examining the head and neck, and taking note of any cuts which might need to be cleaned and closed. They also need to check for objects or debris.
- Checking for any areas where the person can’t feel anything or has less sensation, especially before any surgery. This helps the doctors know about possible nerve damage.
- If the middle of the face has been hurt, it’s common for the person to have less sensation in the part of the face that the second branch of the facial nerve (trigeminal nerve) controls.
- Looking for any unevenness in the face that could show a fracture.
The doctors also have to check the patient’s eyes. They look for any double vision, bleeding under the clear part of the eye, checking how well the person can see, and if they have any trouble moving their eyes. If the doctors have any worries, they will refer this to an ophthalmology specialist. The person might find it hard open their mouth because of swelling caused by a blood collection or because of the lower part of the cheekbone pushing into the jaw joint.
If the cheekbone and the upper jaw are both broken, it’s common for the bottom of the eye socket to also be fractured. This is because it’s quite a thin and weak bone. This can then drain into the sinus in your cheekbone. If it doesn’t, blood and fluid can collect at the back of the eye, causing a retrobulbar hematoma. This requires immediate surgery. A diagnosis of retrobulbar hematoma is usually based on symptoms of a “frozen” eye, and pressure on the eye is usually between 50-70.
If a person has a certain type of fracture named Lefort I, features often include a moveable section of the upper jaw which involves the teeth, a change in how the teeth meet, or damage to the teeth. The upper jaw can be easy to move and very obvious if the person tries to talk. Other types of fractures like Lefort II and III may present with a variety of symptoms, including effects on the eye socket and nasal bones. If the person has a fracture that involves the zygomatic-maxillary complex, they may have symptoms like puffiness, bleeding under the clear part of the eye, bags around the eyes and a sunken eye. Sometimes, they have serious eye injuries. If any eye injuries are suspected, an eye specialist should carefully check them.
A useful hint when checking over the face is to gently wiggle and move any bone parts. This might be mildly uncomfortable for the patient, but combining this with a CT scan is the best method to diagnose fractures in the face, especially in the upper and lower jaws.
Testing for Maxillary Fracture
The first step when evaluating a patient with a suspected facial injury is ensuring they can breathe easily, as these injuries often interfere with the airway. It’s also essential to check for potential spinal and head injuries, especially if the damage was caused by a high-speed impact. A small percentage of individuals with LeFort fractures, a particular type of facial fracture, also have spinal fractures or spinal cord injuries.
An eye examination should also be conducted as part of the initial evaluation. Injuries to the midface region can lead to serious eye issues, including bleeding behind the eye, pressure on the optic nerve, and separation of the retina. Detecting these problems early can call attention to the need for further examination by an eye specialist or even immediate treatment. In fact, there have been cases where eye injuries from midface fractures required surgical intervention by an eye specialist.
Imaging is a crucial part of diagnosing a maxillary fracture, which is a break in the upper jaw bone, and planning its repair. Choices include standard x-rays, CT scans, and MRI scans. The advantage of three-dimensional imaging is that it can show displaced fractures and reveal damage to surrounding structures such as nearby fatty tissue, muscles, and nerves. For certain types of fractures, specific imaging techniques are used. For example, if a break in the zygomatic-maxillary complex, which forms the prominence of the cheek, is suspected, then particular x-ray views are utilized. However, with children, interpreting these types of x-rays can be challenging and might delay the identification of the facial fracture. Hence, CT scans are typically preferred in children.
If LeFort fractures are believed to be present and there’s a possibility that the fracture involves the eye socket or floor, then CT scan is the best choice for imaging.
Overall, CT scans are the best option for detecting fractures. Standard x-rays could be used if a CT scanner isn’t available, but this is not the best first choice. MRIs are seldom used in a trauma setting and aren’t helpful for checking the bones. It’s also critical to get the best possible detail from CT scans. Thin CT slices, often 0.5mm or 0.625mm, from all directions (axial, sagittal, coronal) should be taken, as standard 2.5mm slices from head CTs could miss many fractures. A 3D reconstruction can also help identify fractures that might not be clearly visible in single view slices.
Treatment Options for Maxillary Fracture
For patients with maxillary (jaw) fractures, managing the situation quickly and effectively is key. Sometimes patients may require immediate medical intervention from a resuscitation team, including procedures to open the airway like cricothyroidotomy or tracheostomy. If the patient has fractures in the middle of their face, inserting a breathing tube through the nose can be risky, so care has to be taken to secure the airway without passing the tube between the teeth. This is crucial, especially when planning for future surgery to rebuild the damaged area.
Patients with midface fractures can be managed by experienced anesthesiologists using special fiberscopic equipment for nasal intubation. Alternatively, a submental (under the chin) intubation can be carried out in conjunction with a surgical team. This would involve placing an oral breathing tube, making an incision under the chin, and then pulling the tube through.
The main goals for treating maxillary fractures are to maintain function and appearance. Timing for treatment is important, especially when considering cosmetic outcomes. Immediately after an injury, visual abnormalities may be hard to spot due to swelling. It’s usually best to let the swelling decrease before starting reconstruction surgery.
Non-invasive treatment is recommended for minor fractures that don’t impact function or appearance or in cases where the patient is medically unstable and can’t tolerate general anesthesia. These treatments may include regular pain relief medication, eating a soft food or liquid diet, avoiding further trauma, and refraining from activities that can cause changes in pressure, like blowing your nose.
On the other hand, surgery becomes necessary if there are concerns around the eyes, particularly if there’s a hematoma behind the eyeball that is putting pressure on the optic nerve. Symptoms of this condition may include seeing double, swelling of the eye tissues, or vision loss. Other reasons for surgical intervention include noticeable appearance-related issues and problems with teeth alignment. If the jaw is severely fractured and very unstable, it has to be stabilized and reconstructed.
For Lefort fractures, which are severe facial fractures, treatment focuses on restoring the face’s projection and bite alignment. Surgical management includes limiting jaw movement, exposing the fracture, repositioning the fractured parts, fixating with plates, and repairing the soft tissues. A study conducted in Northeast Iran suggested that open reduction and internal fixation were the most successful treatments, with patients experiencing no complications, such as sensory defects, bite issues, or mouth opening problems. This success was attributed to the technique’s ability to deliver stable and precise anatomical corrections.
What else can Maxillary Fracture be?
When a person has a fracture in their upper jaw, doctors need to consider other potential issues that might have occurred in the head area. These can include injuries to the eye socket (orbital floor), broken teeth (dentoalveolar fractures) or damage to the area that holds the teeth. It might also be possible that there are pooled blood spots known as hematomas, bruising, or swelling caused by the trauma.
What to expect with Maxillary Fracture
The future health outlook of a patient who has suffered a maxillary (upper jaw) fracture is dependent on several elements. These factors include how severe and where the fracture is, any accompanying injuries, and the patient’s ability to breathe properly after the injury.
The patient’s recovery, in terms of functionality and appearance, hinges on the seriousness of the injury, the type of surgery performed, the surgeon’s skill, and the patient’s care after surgery. Generally speaking, a specific type of fracture known as Lefort fractures tend to have a great prognosis when treated with a procedure called open reduction and internal fixation.
Possible Complications When Diagnosed with Maxillary Fracture
A common risk associated with maxillary fractures, specifically Lefort fractures, is death. Studies show that 11.6% of people with Lefort fractures and 5.1% of people with simple midface fractures died. However, the chances of this happening can depend on how the injury occurred, how severe it is, and if there are other injuries present.
Maxillary fractures, including Lefort fractures, are often linked with serious eye problems. Nearly half of the patients (47%) have significant vision issues. Others report seeing double (21%), and having overflow of tears (37%). Additional complications that can occur are:
- Infection
- Difficulty in opening the mouth (trismus)
- Facial nerve issues
- Malunion (improper bone healing), leading to facial asymmetry
- Infraorbital nerve injury, which happens in 30% to 80% of patients suffering from Zygomaticomaxillary complex (ZMC) fractures, causing changed sensation along its route
To avoid complications, good surgical practices and patient education about post-surgery care and follow-ups are vital. Another problem that patients could face is malocclusion, which is a misaligned bite. Despite excellent surgical technique, the patient might feel that the bite is slightly off. This issue can usually be fixed after the surgery by using elastics if arch bars are in place, and if necessary, by consulting with an orthodontist.
Preventing Maxillary Fracture
Taking steps to prevent maxillary fractures, or breaks in the upper jaw, from road traffic accidents could involve using public transport more instead of driving private vehicles. Other measures could include enforcing the use of helmets for motorbike riders and increasing safety regulations for all motor vehicles and motorcycles.
In countries where sports injuries often result in maxillary fractures, encouraging athletes to wear helmets and use mouth guards made by dentists could help minimize both the number and severity of these injuries.
Moreover, it’s worth noting that maxillary fractures are often associated with alcohol and illegal drug use. To address this, increasing taxes on alcohol as well as focusing more on enforcing laws against illegal drugs could be beneficial. Additionally, public health campaigns can educate the public and encourage behavior changes to reduce these risky behaviors.