What is Pronator Teres Syndrome?
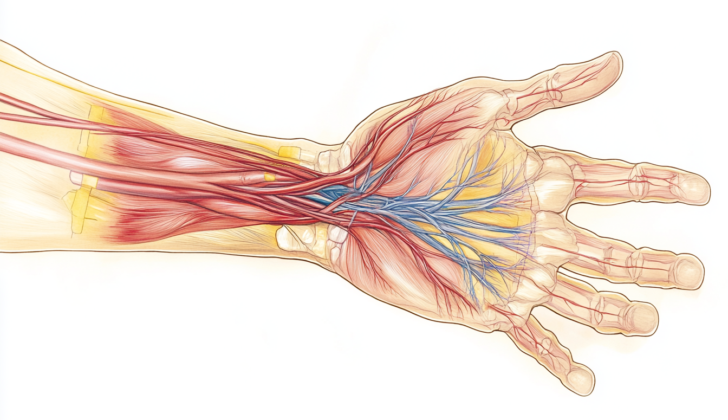
Pronator Teres Syndrome (PTS) is a condition first identified by Henrik Seyffarth in 1951. It’s caused by the Pronator Teres muscle in your forearm pinching the Median Nerve. The Pronator Teres muscle is so named because it helps turn the forearm and has a rounded shape. In most cases (66%), it’s made up of two unequally sized parts: the larger part is attached to the upper inside part of your upper arm bone, and the smaller part is attached to a bony protrusion of your ulna, one of the two bones in your forearm. These two parts come together to form a common flexor tendon that attaches to the shaft of your radius, the other bone in your forearm. The Median Nerve, which controls both these parts, passes between this muscle group in 74% to 82% of cases. This nerve originates from the C6-7 roots in your spinal cord. In rare cases (14%), the smaller part of the muscle is missing, which may lower the risk of the Median Nerve being pinched. Many people also have extra fibrous bands within the Pronator Teres muscle. Further down the arm, the Median Nerve splits to form the Anterior Interosseous Nerve about 5 to 8 cm away from the inside part of your elbow.
What Causes Pronator Teres Syndrome?
Pronator teres syndrome is a condition that can develop from quick and repetitive hand motions such as prolonged hammering, scooping food, washing dishes, or playing tennis. These actions may cause the pronator teres muscle in your forearm to thicken, potentially trapping a nerve, especially in people who have additional fibrous bands in their arm.
This syndrome can also arise after a local injury, or due to a specific type of tumor called a schwannoma that compresses on the nerve. It has also been seen in patients undergoing treatments like blood thinning therapy and kidney dialysis.
Another factor that can make the symptoms of pronator teres syndrome more severe is a tight lacertus fibrosis, also known as the bicipital aponeurosis. This is basically an extra layer of tissue in your arm that’s located near the bicep muscle.
Risk Factors and Frequency for Pronator Teres Syndrome
Pronator teres syndrome is an uncommon condition that often gets confused with the more common carpal tunnel syndrome. No specific age group is more likely to have it, but some studies suggest it may be more common in men.
Signs and Symptoms of Pronator Teres Syndrome
Pronator teres syndrome is a condition that often causes pain in the inner forearm. The pain usually gets worse when you try to turn your forearm inwards or bend your elbow. You might also feel a tingling sensation, known as a Tinel sign, over the inner edge of your upper forearm.
Some people with pronator teres syndrome also report feeling noticeably weak. While it’s rare for the muscles supplied by the median nerve to waste away, it’s not unusual for the thumb’s long flexor muscle and the thumb’s short abductor muscle to be slightly weaker than normal. These muscles help you move your thumb, and the muscles that help you move your fingers 2 and 3 can also be affected. However, the pronator teres muscle itself usually remains unaffected because it gets its nerve supply before the median nerve passes through it.
The condition can cause varying levels of sensory loss, which can affect your palm or have symptoms similar to carpal tunnel syndrome. This includes areas like the fleshy part of your thumb, your thumb, your index and middle fingers, and your ring finger. Some people can have a positive Phalen test over the pronator teres muscle, which is a test for carpal tunnel syndrome, in half of the cases.
- Pain in the inner forearm
- Increase in pain when the forearm is turned or the elbow is bent
- Tingling sensation over the inner, upper forearm (Tinel sign)
- Weakness in the hand and fingers
- Weak thumb movement
- Possible sensory loss in the palm or fingers
- Positive Phalen Test for some individuals
Testing for Pronator Teres Syndrome
Pronator teres syndrome, a condition that affects the nerves in your arm, is often tested with something called nerve conduction studies (NCS). These studies help doctors rule out other similar conditions that affect the nerves. However, these studies don’t always show abnormalities, particularly for pronator teres syndrome. They mainly show that amplitudes, the measurement of the electric signals in your nerves, may be reduced more than the speed at which these signals are transmitted (the conduction velocities). This is especially true for patients who have severe symptoms and damage to the axon, the long, threadlike part of a nerve cell.
Another diagnostic test used is electromyography (EMG). This test measures the electrical activity of muscles. In pronator teres syndrome, abnormalities are often found in certain forearm and hand muscles (like the FPL, FDP to digits 2 and 3, FDS, and APB). It’s uncommon, though, to find abnormalities in the PT muscle.
If any of the muscles show abnormalities, your doctor will also test other muscles supplied by a different nerve but controlled by the same region of the spinal cord (myotomes). This is to check if there are issues in other areas, like the brachial plexus or cervical roots. However, only about 10% of pronator teres syndrome diagnoses show these abnormal electrodiagnostic findings.
Imaging tests like ultrasound and magnetic resonance imaging (MRI) can also be used to diagnose pronator teres syndrome. Ultrasounds can be a fantastic tool because they allow doctors to view your muscles and nerves in real-time and are usually more affordable than MRIs. Some research findings suggest that the size of the median nerve (the nerve affected in pronator teres syndrome) seen in ultrasound images can give information about the seriousness of the condition, how long it’s been present, and if there is nerve conduction failure.
Treatment Options for Pronator Teres Syndrome
If you’re experiencing symptoms, there are two main ways to manage your situation: conservative or non-surgical treatments, and surgical treatments.
Non-surgical treatment is often the first step. This includes resting, changing activities that worsen the symptoms, going for physical and occupational therapy, taking anti-inflammatory medications, and getting small, localized injections with medicines to reduce inflammation or numb the area. These strategies can allow you to keep working, unless you’ve lost a significant amount of feeling or strength, which might limit your ability to do your job. You’ll usually try non-surgical treatments for at least 6 weeks. If these efforts aren’t successful, your doctor might then consider surgery.
Surgery typically becomes an option if you have ongoing symptoms, your doctor finds evidence of weakness or muscle shrinkage during a physical exam, and tests show abnormal results. The surgery often involves exploring and releasing different areas in the forearm that might be putting pressure on the nerves. This can include parts of muscles and other structures. Sometimes, the surgeon might need to decompress or relieve pressure on the nerves at multiple places, but this is still considered a single procedure.
An endoscopic release is a type of surgery that has several advantages over traditional open surgery. First, it doesn’t disrupt the blood supply to the nerve. It also results in less scarring. People have reported great outcomes with this approach. However, if your symptoms come back after surgery, a more traditional open surgery might be needed.
What else can Pronator Teres Syndrome be?
: When a person has symptoms similar to the Pronator Teres Syndrome, doctors also consider the possible presence of the following other conditions that affect the same nerve in our body called the Median Nerve:
- Ligament of Struthers Entrapment: This condition is caused by a ligament compressing the median nerve. This is seen in 1-2% of people. Pain in the forearm and tingling in the fingers are common symptoms that increase with turning the forearm upwards and straightening the elbow.
- Other Median Nerve issues: The median nerve can also face pressure because of a thickened Lacertus Fibrosis (a tissue connecting the biceps muscle to the forearm) or the Sublimis Bridge (a part of a forearm muscle). These conditions worsen with resistance to bending of the elbow or fingers.
It’s vital to note that Pronator Teres Syndrome should be differentiated from Carpal Tunnel Syndrome, which affects the wrist. The symptoms can overlap, and sometimes both conditions can occur together, often leading to a misdiagnosis.
The symptoms of Pronator Teres Syndrome are different from Carpal Tunnel Syndrome in several ways. In Pronator Teres Syndrome, the entire area supplied by the median nerve experiences a loss of sensation, whereas in Carpal Tunnel Syndrome, a part of the hand retains its sensation. Also, patients with Pronator Teres Syndrome do not usually have wakefulness due to tingling sensations at night.
The Pronator Teres Syndrome should also be considered when a patient with Carpal Tunnel Syndrome does not improve after surgery.
Moreover, these conditions should also be distinguished from anterointerossenus nerve syndrome, brachial plexus injury, or neck-related nerve pain. An examination revealing weakness in areas not related to the median nerve or neck pain radiating to the arm suggest these conditions.
Yet another condition to consider could be Neuralgic Amyotrophy. Though similar to Pronator Teres Syndrome, this usually affects multiple nerves and improvement is often observed after six to twelve months.
What to expect with Pronator Teres Syndrome
Pronator teres syndrome is a condition where a muscle in the forearm traps a nerve causing discomfort. The good news is that most patients recover well from this after a procedure to release the muscle. Typically, they’re able to return to less strenuous duties in about 3 weeks, and their regular routine in about 6 weeks.
Occupational therapy can speed up recovery and is especially important for patients who’ve had tendon transfers or still feel weak even after the treatment. For these patients, they may be able to go back to less strenuous duties in about 6 to 8 weeks, and their regular work routine in about 10 to 12 weeks.
Possible Complications When Diagnosed with Pronator Teres Syndrome
Surgical treatment for conditions like pronator teres syndrome generally has a low risk of complications. In one study involving 72 patients, there were no recorded complications during the surgery. Moreover, 59% of the patients were either quite happy or satisfied with the postoperative results.
However, there is a theoretical risk of the following complications after surgery:
- Infection
- Buildup of lymph fluid or blood outside of blood vessels (Seroma/hematoma formation)
- Nerve damage
- Scarring
Preventing Pronator Teres Syndrome
When doctors recommend a careful approach to treatment, they often advise patients to reduce the amount of time they spend on activities that require a lot of turning or twisting of the forearm. Doing these activities often could slow down recovery or worsen the condition. These activities include:
- Using a hammer
- Serving food with a ladle
- Washing dishes
- Playing tennis
- Pouring drinks, which is something waiters and bartenders do a lot
- Carrying books, which is something librarians do frequently
- Twisting clothes, like when you’re wringing them out
By limiting these activities, you help your body heal and prevent further injury.