What is Chondrodermatitis Nodularis Helicis?
Chondrodermatitis nodularis helicis, or CNH for short, is a common and non-dangerous condition that causes inflammation in the skin and cartilage of the ear’s outer part, also known as the pinna. It’s also known as Winkler disease, named after the Swiss dermatologist who first detected it back in 1916. While it usually affects the outer edge of the ear, it can occasionally affect the inner edge, leading some to propose a name change to chondrodermatitis nodularis auricularis. Other names for this condition are nodular chondrodermatitis and chondrodermatitis nodularis antihelicis.
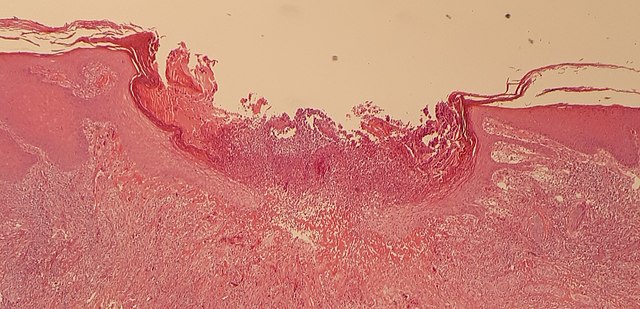
The condition leads to a noticeable bump on the ear and is often accompanied by pain. Due to these symptoms, doctors might take a biopsy to rule out skin cancer, such as squamous cell carcinoma. However, under microscopic examination, CNH is clearly different from skin cancer, regardless of how similar they might look to the naked eye.
The condition may occur due to pressure on the ear and can worsen due to various factors. Ear pain, specifically around the outer edge of the ear, is a common symptom. Treatments typically start with measures to reduce pressure on the ear. Surgery to remove the problematic lump is only considered as a last resort. It’s important for healthcare professionals to be able to quickly identify and treat this condition to ensure good outcomes for patients.
What Causes Chondrodermatitis Nodularis Helicis?
The exact cause of CNH, or chondrodermatitis nodularis helicis, isn’t entirely known. However, most researchers think it’s due to put excessive and consistent pressure on the ear, particularly the outer part called the pinna. Habits like sleeping on the same side every night or prolonged use of headphones, hearing aids, or other headgear that exert constant pressure on the ear may play a role in causing the condition.
CNH can also be linked to autoimmune and connective tissue disorders, particularly in young women. Other possible contributing factors are certain physical features of the ear such as a prominently sticking out helix (outer edge) or antihelix (inner ridge). Moreover, issues like recurrent injury to the ear, past surgery, radiation damage, sun exposure, and cold weather exposure could also play a part in causing CNH.
The specific structure of the pinna or the outer part of the ear makes it susceptible to CNH. It has minimal underlying soft tissue and a limited blood supply, which makes it prone to damage from pressure and cold. Given the thin skin and scarce soft tissue of the pinna, and its position on the side of the head limiting its blood supply, healing may take longer and chances of inadequate blood supply (ischemia) may increase.
Risk Factors and Frequency for Chondrodermatitis Nodularis Helicis
There isn’t a lot of information available about CNH (chondrodermatitis nodularis helicis), so its exact incidence is still unknown. What we do know is that it tends to affect middle-aged or older men more often. However, women and young adults can also get it, while it’s quite rare in children. People from all ethnic groups can develop CNH, but it seems to more commonly impact those with fair skin who have been exposed to the sun excessively over time.
- CNH often happens but isn’t well-documented or studied, hence the exact number of cases is unclear.
- Without any association with autoimmune disorders, the condition is more common in middle-aged or older men.
- Even though rare, women and younger adults can also have CNH, and it’s very rare in children.
- CNH can affect all ethnic groups, but people with fair skin who often spend a lot of time in the sun are more susceptible.
Signs and Symptoms of Chondrodermatitis Nodularis Helicis
People with Chondrodermatitis Nodularis Helicis (CNH) typically complain about a painful bump on the outer ear. This usually occurs without any known history of ear injury. It most commonly develops on the ear that people sleep on and is more likely to be found on the right ear in men and the left ear in women. While the bump typically only shows up on one side, it can occur on both ears. Factors like having protruding ears, using headgear or hearing aids, frequent phone use, and a predisposition to autoimmune conditions may contribute to the development of CNH.
The lump may grow quickly at first, but usually stops enlarging after a certain point. The most common symptom is pain at night. In some rare cases, people have reported experiencing pain during the day, usually if the bump comes into contact with something.
A physical examination usually reveals a noticeable, rounded bump with a crusty center, often located over an ulcer that may lay bare some cartilage at the bottom. Sometimes, the lump may be flat or appear to be attached to the surrounding skin due to scarring. The bump is often 4 to 6 mm in diameter and may be surrounded by a reddish area, especially if it’s painful. The most common location for these lumps is at the top of the ear. The lump is typically firm, tender, and generally attached to the underlying ear cartilage. Other features can include bleeding and fluid buildup after the crust is removed. It’s more common for women to develop CNH on the inner curve of the ear. In some rare instances, the bumps can appear on other parts like the outer ear canal and the back of the ear.
Testing for Chondrodermatitis Nodularis Helicis
Diagnosing Collapsing Neuropathy or CNH usually starts with a clinical examination, where the doctor checks the patient physically. To affirm the diagnosis, a skin biopsy (where a small piece of skin is extracted and analysed) may be performed.
Some medical experts also advise conducting laboratory tests to exclude the presence of body-wide illnesses like dermatomyositis, scleroderma, thyroid disorders, and other diseases related to the body’s connective tissue (collagen vascular diseases). This is particularly true for adults below the age of 40.
Treatment Options for Chondrodermatitis Nodularis Helicis
There are a number of ways to manage CNH, or chronic pain in the ear. These are generally divided into two categories: non-surgical treatment and surgical removal.
The first option for treatment can include pressure-relieving padding or prostheses. These are cheap and easy to use, with the primary goal of relieving the pressure on the affected area. These pressure-relief options come in many forms, such as adhesive foam sponges, foam bandages strapped to the head, and special pillows designed for sleeping. Their success varies, mainly based on how well the patient follows the treatment plan, but they can be up to 87% successful.
Some doctors have tried using topical and injected steroids for treatment, but these do not seem to be effective on their own if the pressure on the site isn’t addressed as well. Injecting a substance called hyaluronic acid into the affected site could provide relief by cushioning the area.
Other available treatments include photodynamic therapy, which may require multiple sessions, and argon or carbon dioxide laser treatments, which effectively blast away the lesion allowing the wound to heal naturally. This approach is an alternative to conventional surgery.
Topical treatments such as 2% nitroglycerine paste applied twice daily can improve symptoms by increasing blood flow to the affected area. Nitroglycerine patches or a topical cream called diltiazem can also be effective. Liquid nitrogen can be used to freeze off the lesion, and electrocautery, or using electrically heated instruments, can remove the lesion and is another alternative to surgery.
When it comes to surgical treatment, there are many approaches. These include cutting out a wedge of tissue surrounding the lesion and reconstructing the area, removing the skin and cartilage of the lesion, and sparing the skin while just removing the cartilage. The simplest method, which involves surgical removal and careful trimming of cartilage, is typically recommended and provides good results. However, there is a chance of the CNH coming back, with recurrence rates up to 30%. A less invasive technique involves using a special tool to remove the lesion and then applying a small skin graft to the wound. This approach has a reported recurrence rate of 17%.
What else can Chondrodermatitis Nodularis Helicis be?
Chondrodermatitis nodularis helicis (CNH) can often be mistaken for serious skin conditions like basal cell carcinoma because they look similar – both present as nodules, or small bumps, with a crusty center. If CNH gets bigger and inflamed, it could be confused with squamous cell carcinoma as well. Another condition that could be mistaken for CNH is ‘gouty tophi’ – but unlike CNH, gouty tophi usually show up as multiple bumps and are more likely to appear on the fingers and toes.
One more skin condition that might look initially like CNH is ‘keratoacanthoma’. Yet, keratoacanthoma generally grows much faster and typically disappears on its own after a few months – this is because it grows so fast that it outpaces its own blood supply! Unlike keratoacanthoma, CNH isn’t likely to go away without treatment.
CNH patches with a lot of keratosis, or skin cell build-up, may look like either seborrheic dermatitis (red, greasy, flaky skin), keratotic dermatitis (hard, rough, and possibly itchy skin), or verruca vulgaris, also known as common warts.
What to expect with Chondrodermatitis Nodularis Helicis
CNH generally has a positive outlook, though it usually takes months to recover using non-invasive measures. It’s incredibly uncommon for it to go away on its own. Also, there’s a higher likelihood of CNH coming back if the necessary changes to daily habits are not kept up.
Possible Complications When Diagnosed with Chondrodermatitis Nodularis Helicis
CNH, or nodules on the skin that can be painful, usually doesn’t get better without treatment. It also tends to stay in a small, well-defined area, usually no bigger than 4 to 6 mm. Despite this, not treating the nodules doesn’t tend to cause other long-term problems. However, the patient might experience lack of sleep and constant discomfort because these nodules are quite uncomfortable.
Unfortunately, there’s a chance of infection if the skin gets damaged and exposes the tissue underneath. Treatment, especially surgery, might not always work as well. The area might not heal properly, or it might not solve the issue. If surgery leaves an edge or point on the tissue, applying pressure might even lead to new nodules.
Preventing Chondrodermatitis Nodularis Helicis
While doctors don’t need to advise all patients about the importance of changing sleeping positions at night to prevent the onset of a skin condition known as CNH, it is key for primary care providers to understand this condition. Doctors should be quick to recommend patients avoid putting stress on their ears if they start noticing painful spots with crust in the center appearing on the curves of their ears. A lot of cases of CNH can successfully be treated with simple measures over several months.
Ways to treat this condition might include taking a break from wearing helmets or hearing aids, using alternative methods to hold your phone during calls, shielding the ears from cold weather, and changing your sleeping habits, such as sleeping on a different side or using a doughnut-shaped pillow. These small changes can help significantly in curing CNH.
Furthermore, it is critical to promptly consider a biopsy for these skin conditions, especially if they aren’t causing pain. This is because they tend to show up in areas that are susceptible to non-melanoma skin cancer. This is particularly common in men over the age of 40 who have a history of skin damage from sun exposure.