What is Posterior Hip Dislocation?
In the US, hip dislocations cause a lot of physical harm and could possibly result in death. They can also damage the surrounding body structures, nearby joints, and a person’s ability to move around normally.
When examining a posterior hip (at the back of the thigh) dislocation, it’s important for the doctor to first determine if the hip joint is an original or a replacement, as different treatment approaches apply. They must also check for other injuries like fractures, which could greatly change the way the condition is managed.
An original hip joint is usually very stable and would need a lot of force to become dislocated. Because of this, hip dislocations in original joints usually happen because of traumatic events like car accidents. But this isn’t surprising given that, of those who have a hip dislocation from a car accident, 95% also had another injury that needed hospital care. Consequently, a comprehensive examination of the nerves and muscles, as well as x-ray or CT scans, are necessary for assessing a dislocated original hip joint.
On the other hand, dislocations in replaced or non-original hip joints are quite common in emergency departments across the country. This is because these joints are inherently less stable than original ones. These types of dislocations are most often connected with minor incidents and usually need less aggressive treatment approaches.
What Causes Posterior Hip Dislocation?
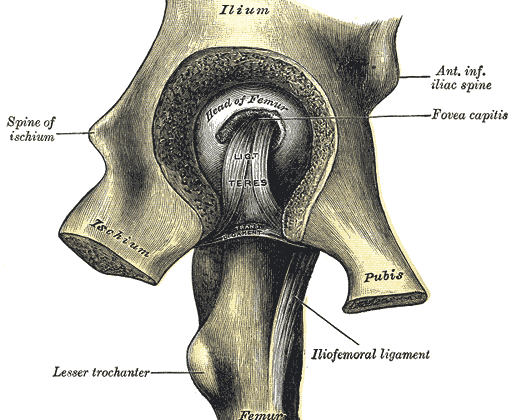
Hip dislocations can either be anterior, meaning the hip is displaced forward, or posterior, where the hip is displaced backward based on what causes it. In the case of posterior dislocations, the ball-like top of the thigh bone, or femur, moves back out of the hip socket when the hip bends, moves inward and rotates inward. Conversely, during an anterior dislocation, the femur tends to pop forward out of the hip socket when the hip stretches too far back and to the side. Most unusual and intense injuries often result in a posterior dislocation.
Risk Factors and Frequency for Posterior Hip Dislocation
Age, race, and gender can increase the chance of certain injuries, with women being twice as likely to experience them than men. The most common type of these is the posterior hip dislocation, which makes up 90% of occurrences. Additionally, these dislocations can be associated with severe health risks if they result in fractures. Dislocations can cause a great deal of pain and come with other problems such as fractures in the hip area, bone death, nerve damage, repeated dislocations, bone bruising, tears in the inner knee, and others. There is also a 8% chance that a thoracic aortic injury might occur with a posterior hip dislocation as a result of sudden, abrupt deceleration injuries.
After a dislocation, doctors typically try to fix the problem with a closed procedure while the patient is sedated. This immediate correction is particularly vital for original hip joints to reduce the risk of bone death. If this approach doesn’t work, an orthopedic surgeon will use open surgery to fix the dislocation. Regardless of the method used, the patient must strictly follow precautions to stop the hip from dislocating again and avoid more injury. If the hip keeps dislocating, the patient might have to wear a brace or undergo additional corrective surgery.
- Age, race, and gender are important factors in the risk for certain injuries, with women being twice as likely to experience them than men.
- Posterior hip dislocations are the most common type, accounting for 90% of all dislocations.
- These dislocations can pose significant health risks, especially if associated with fractures.
- Dislocations can cause various symptoms, including severe pain, fractures, bone death, nerve damage, repeated dislocation, bone bruises, knee injuries, and more.
- There’s a chance that a thoracic aortic injury might occur with a posterior hip dislocation.
- Doctors usually try to correct a dislocation immediately through a closed technique. If this doesn’t work, open surgery is conducted.
- Patients must strictly follow precautions after the procedure to prevent future dislocations and further injury.
- Continual dislocations might require the patient to wear a brace or undergo more corrective surgery.
Signs and Symptoms of Posterior Hip Dislocation
Posterior hip dislocation is an injury that is typically easy to diagnose because it causes a lot of pain, and the person with this injury can’t walk or bear weight on the injured leg. Generally, the person may report a significant “clunk” or “popping” sound right before the pain began. They likely also have a noticeable change in the appearance of the hip, with the hip being visibly shorter, more flexed, moved closer to the center of the body, and turned inward. It’s also crucial to check the pelvis and the same side knee. Whenever needed, emergency care principles like those in the ATLS program should be used. It’s also important for a thorough check of nerve and blood vessels to be done when the person first arrives, and again before and after the hip is returned to its normal position. This check should be repeated regularly, to track any changes.
Indicators of nerve and blood vessel damage can include:
- A buildup of blood at the site of the injury.
- Pain in the buttock, back of the thigh, and leg.
- Changed feeling in the back of the leg and foot.
- Weakness or even complete loss of the ability to lift the foot up (caused by damage to the peroneal branch of the nerve) or point the foot down (caused by damage to the tibial branch).
- Reduced or lost reflexes at the ankle.
Testing for Posterior Hip Dislocation
After a detailed check-up and physical examination, the doctor may decide to take images of the affected joint.
The first step is usually a standard x-ray of the pelvis from the front. Doctors look for several smooth, unbroken lines on this x-ray which can indicate whether the structure of your hip is normal or not. Special attention is given to the back wall of the hip socket, as fractures here are common when the hip dislocates. The x-ray can also determine the presence of a femur fracture and its location as well as if one side of the hip appears smaller than the other.
A side view x-ray can be done to determine the direction of the hip dislocation. More targeted x-ray views might be done to identify fractures in the hip socket.
A type of scan called a Computed Tomography (CT) is then done for everyone with a traumatic hip dislocation. This scan helps to see in more detail if there are any associated fractures and how extensive they are. It can also highlight any trapped bone fragments.
Magnetic Resonance Imaging (MRI) is not usually employed routinely. However, it can be useful in checking for injuries to soft tissues, such as the labrum and cartilage. It is usually preferred for children because their bones are still growing.
Treatment Options for Posterior Hip Dislocation
The treatment of posterior hip dislocations involves either operative or non-operative methods, all of which aim to put the hip back into place as soon as possible. Research indicates that the longer the hip remains dislocated, the higher the risk of complications such as avascular necrosis (dead bone tissue due to inadequate blood supply). Experts typically recommend that the hip is repositioned within six hours, though evidence also suggests that this action may be critical within twelve hours. It is important to note that complications increase significantly with an extended dislocation time.
Non-Surgical Management
Non-surgical techniques have been developed to put a dislocated hip back into place without any surgical intervention. The following are different techniques that can be used:
- Allis Maneuver: Essentially, the knee is bent at a 90-degree angle while traction (pulling) and flexion (bending) are applied to the hip until it’s back in place.
- Bigelow Maneuver: Here, the hip is flexed at 90 degrees and then manipulated into place using different movements.
- Lefkowitz Maneuver: The doctor uses their knee to support the patient’s bent knee and maneuver the hip back into place.
- Captain Morgan, East Baltimore Lift, and Howard techniques: These methods involve various ways of applying pressure and movement to reposition the hip.
- Lateral Traction, Piggyback, Tulsa, Rochester and Whistler Techniques: These named maneuvers involve the use of traction (pulling force) along with other movements to reduce the dislocation.
In any case, an X-ray should be performed after the hip is repositioned to ensure it is in the right place. A CT scan may also be necessary for some patients to check for other injuries. Weight-bearing activities such as standing or walking may need to be limited for 4 to 6 weeks after the reduction.
Surgical Management
If non-surgical attempts to reposition the hip fail, surgery may be required. Other reasons for surgical intervention may include a fracture in the femur, disruption in the hip due to bone fragments or soft tissue, or if there is a need to fix a fracture in the nearby area. Surgery allows for the removal or repair of any fractured bone pieces and can also be used to examine and repair soft tissues. The surgical approaches for repositioning a dislocated hip include the Kocher-Langenbeck (from the back) approach or the Smith-Peterson (from the front) approach.
What else can Posterior Hip Dislocation be?
- Bruises
- Decreased blood supply causing damage to the thigh bone head
- Break in the neck of the thigh bone
- Injuries and breaks in the thigh bone
- Break in the hip bone
- Injury to the hip from a hard impact
- Condition causing the hip bone to slip at the growth plate
- Condition causing a snapping or popping sound in the hip during movement
- Partial dislocation of the hip due to an injury
What to expect with Posterior Hip Dislocation
Simple dislocations usually result in quicker recovery and better outcomes. The more complicated the dislocation, the higher the chances of complications. Many factors can affect prognosis, but the most critical one is how quickly the injury is treated. Early treatment usually leads to better outcomes.
Other factors that can influence recovery include the type of fracture-dislocation, how well the hip joint fits together after treatment, and the severity of the injury.
Possible Complications When Diagnosed with Posterior Hip Dislocation
There are several complications that can occur after a posterior hip dislocation. These include:
- Lack of blood supply to the head of the thigh bone, also known as avascular necrosis of the femoral head
- Chondrolysis, or the breakdown of cartilage
- Increased risk of arthritis after trauma, especially in more complex dislocations
- Damage to the sciatic nerve
- Abnormal formation of bone in muscle tissue, known as heterotopic ossification
- Chances of the hip dislocating again
Studies have shown that these complications are more common in severe cases of hip dislocation, known as Thompson-Epstein type IV. Informing such patients about the potential complications can help them understand their condition better. Additionally, the severity of complications like the lack of blood supply to the head of the thigh bone and arthritis increase with the severity of the trauma. These complications are also more common if the hip is not relocated back into place within 12 hours.
In medical studies, it has been recorded that around 10% of adults and 5% of children suffer from sciatic nerve damage after a posterior hip dislocation, and usually, it’s the peroneal branch that gets affected. Fortunately, partial recovery occurs in about 60% to 70% of patients, regardless of the type of injury or treatment received.
Recovery from Posterior Hip Dislocation
If a hip has been successfully put back in place, it’s important to rest, use ice, take anti-inflammatory and pain medications in the immediate aftermath. The degree to which a person can put weight on the hip depends on the severity of the dislocation. For mild dislocations (type I posterior dislocations), patients can start putting weight on it as soon as it doesn’t cause pain. For more severe dislocations (type II to V), it’s best to limit weight-bearing for 4 to 6 weeks.
If the dislocation is complex and comes with fractures or instability, a special brace might be needed after surgery. This brace, known as an abduction brace, keeps the hip stretched out and slightly rotated, while still allowing for controlled movement.
A week after the hip has been put back in place, the patient can start doing gentle exercises, like pendulum movements and passive range of motion movements. As they progress, more advanced exercises can be gradually introduced, such as upright knee raises and resistive hip abduction. A physiotherapist will provide more detailed instructions for these exercises.