What is Posterior Shoulder Dislocations?
The shoulder is a complex joint that connects the arm to the main body structure. Out of all the joints in the body, the shoulder’s glenohumeral joint is the one most often dislocated, making up about half of all serious dislocations treated in emergency rooms. Dislocations that happen towards the back of the shoulder make up 2% to 5% of all shoulder dislocations. In about 30% of patients, repeated back-of-the-shoulder dislocations can lead the joint to deteriorate over time. Diagnosing these kinds of dislocations can be tricky, so it’s important to be particularly alert when you see the usual symptoms and history during an examination.
What Causes Posterior Shoulder Dislocations?
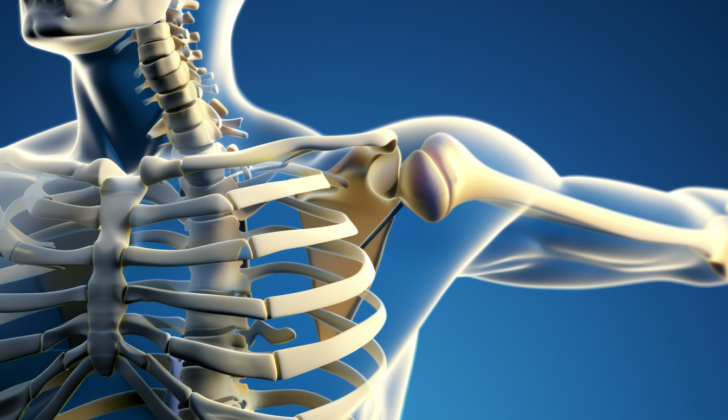
The shoulder is made up of a complex structure which includes a joint known as the glenohumeral joint, a type of ball and socket formation. This is formed by the humeral head (part of your upper arm bone) fitting into a shallow socket in your shoulder blade known as the glenoid fossa. Because the socket is quite shallow and much smaller than the humeral head, the shoulder is capable of a wide range of movement, more so than any other joint in the body.
However, this flexibility also makes the shoulder unstable and more prone to injury, including dislocation. To help with this, the shoulder has a rim of cartilage, called the labrum, around the socket. This deepens the socket and, together with the joint capsule, ligaments, and muscles, helps to stabilize the joint.
The nerves and blood vessels of the shoulder, belonging to the network known as the brachial plexus and the subclavian vessels, run across the front of the shoulder between the first rib and collarbone. While these can be injured, it’s less common for them to be damaged by dislocations at the back of the shoulder.
A shoulder can dislocate due to various types of injury, such as a hard hit, a blunt force, or a twisting movement. The most common cause is a forceful movement where the arm is pressed inwards and rotated internally. A direct, blunt hit to the front of the shoulder can also result in dislocation. If someone dislocates their shoulder at night for no apparent reason, it could be a sign that they’ve had a seizure.
Risk Factors and Frequency for Posterior Shoulder Dislocations
Shoulder problems and dislocations can occur in all adults, no matter their age or gender. Older people can often experience more connected issues like injuries to the soft tissue and instability after a dislocation, including damage to the rotator cuff. So, it’s essential to provide them proper medical care and follow-up.
Signs and Symptoms of Posterior Shoulder Dislocations
If you’re experiencing problems with your shoulder, it’s important to provide your doctor with as much information as possible. Doctors usually need to know your age, which arm you mainly use, where you feel pain and how severe it is, when the injury happened, conditions that make the pain worse or better, whether the pain spreads to other areas, and how the injury occurred. For an effective examination, you need to undress to expose both shoulders for a thorough inspection.
Range of motion tests are performed to see how far inwards and outwards you can rotate your shoulder and how far you can lift up and lower down your arm. It’s worth noting that about 50% of dislocations towards the back of the shoulder may be overlooked during the initial evaluation. During the exam, the doctor will check for any related nerve or blood vessel injuries.
The front, side, and back of your shoulder will be inspected and touched to check for signs like a bump in the shoulder towards the backside with a loss of the usual shape towards the front, along with a noticeable protrusion of shoulder sections called the coracoid and acromion. Your arm is often held close to your body with a slight turn inwards. You might not be able to rotate your arm outward or lift it up due to intense pain.
Testing for Posterior Shoulder Dislocations
Before and after X-rays are standard when looking at a dislocated shoulder. When there’s been a substantial injury, dislocation and fracture-dislocation can appear quite similar during a physical examination. X-rays after the shoulder has been repositioned are essential to make sure the shoulder is back in place properly and to check for any additional injuries or fractures during the process. In very special cases of chronic dislocation that happened without a traumatic event, X-rays might not be necessary.
A standard assessment of a painful shoulder typically involves three different X-ray views. Front (anterior-posterior or AP) and “Y” view X-rays are used to check for dislocations toward the back of the shoulder; however, these can often be missed on standard front view X-rays. Therefore, the “Y” view can help to confirm the diagnosis, with the upper arm bone positioned behind the socket at the center of the ‘Y’ shape on the shoulder blade. However, this view can sometimes be obstructed by the soft tissues of the upper arm and the complex bone structure of the shoulder blade and ribs. The side view from the armpit area is the most accurate X-ray picture for diagnosing a shoulder dislocation toward the back. This X-ray gets rid of most other bones and soft tissues that could hide the relationship of the upper arm bone and socket.
On front view X-rays, the upper arm bone can usually be seen turned inward, this makes the top of the upper arm bone look symmetrical, a bit like a light bulb or drumstick. A ‘rim sign’ is when the space between the surface of the upper arm bone and the front rim of the socket is more than 6mm. On occasion, a ‘trough sign’ is seen as a dark line on the inner aspect of the upper arm bone, indicating a compression fracture. It’s also important to check for a reverse Hill-Sachs deformity, a common fracture with back shoulder injuries occurring on the front side of the upper arm bone, which might lead to long term pain, and ultimately, bone death.
A CT scan might be considered if X-rays do not show a suspected dislocation toward the back. Recently, ultrasound examinations performed bedside have also been successfully used to accurately diagnose dislocations. However, they are limited in diagnosing fractures.
Treatment Options for Posterior Shoulder Dislocations
Posterior dislocations, commonly related with intense pain and muscle spasms, often require procedural sedation to be managed. Pain relief methods such as injecting local anesthetics like Lidocaine or Bupivacaine at the joint site are also used to make the reduction process easier.
Closed reduction, a common procedure to fix dislocated joints, involves exerting steady pulling force on the affected arm that is positioned inwards and towards the body. This force along with gentle, frontward motion on the head of the upper arm bone guides it back into the socket. Counter-pressure can be provided by a sheet wrapped around the dislocating arm. Avoiding forceful outward rotation is necessary as it can cause much stress on the upper arm bone, leading to a break.
A successful reduction can be noticed when a “clunk” sound is heard, pain eases, and the patient is able to touch the opposite shoulder with the injured arm’s hand. If this method fails, an orthopaedic specialist should be consulted for an in-depth procedure, and sometimes, surgical correction.
After the reduction, it is important to reassess the blood supply and nerve function. Post-reduction x-rays are beneficial to confirm and document successful reduction and identify any injuries caused during the procedure. Patients should keep their shoulder rested in a sling or shoulder immobilizer, positioned slightly outward and away from the body for some weeks. An early follow-up with an orthopedic specialist is crucial for ensuring proper healing, early range of motion, and rehabilitation.
In cases that are diagnosed late or endure over a long period, it’s necessary to consult an orthopedic specialist. These patients often require surgical correction or even joint replacement. Early surgical repair may lower the chances of the dislocation happening again.
What else can Posterior Shoulder Dislocations be?
When diagnosing a dislocated shoulder at the back (posterior), the doctor needs to consider other possible health issues that can cause similar discomfort, such as:
- Injury to the acromioclavicular joint, which is located at the top of the shoulder
- Inflammation of the tendon attached to the bicep muscle, known as bicipital tendonitis
- Broken collarbone, or clavicle fractures
- Injury to the rotator cuff, a group of muscles and tendons that surround the shoulder joint
- Shoulder dislocation, which can occur at the front or back of the shoulder
- Swimmer’s shoulder, a common injury in swimmers due to overuse or poor technique
Doctors have to carefully consider these potential issues and conduct the necessary tests to make a correct diagnosis.