What is Peroneal Nerve Injury?
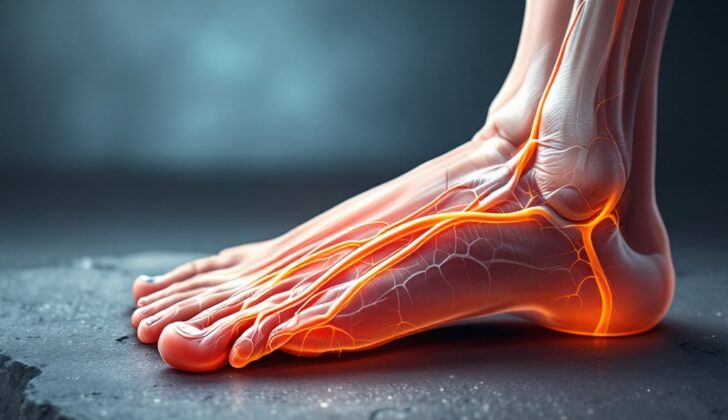
The peroneal nerve, also known as the fibular nerve, plays a crucial role in feeling and movement in your lower leg. These nerves begin in the lower part of your spine, combining to form the sciatic nerve which splits into two primary parts; the peroneal and tibial nerves. These are located at the back of your thigh, near your knee. The peroneal nerve then goes behind a major muscle in your thigh, wraps around the side of your knee, and runs down the outer part of your calf. This nerve divides into two branches and provides sensation and controls movement for different parts of your foot and leg. Understanding these movements and sensations can help spot issues before they serious problems.
The peroneal nerve is responsible for both feeling and action. Movement controlled by the deep branch of the peroneal nerve allows you to flex your foot and extend your big toe. The superficial branch of the nerve helps in twisting your ankle outward. In terms of feeling and sensation, the superficial branch covers the top of your foot except the skin between your first and second toes, which is the responsibility of the deep branch.
If your peroneal nerve gets damaged, it can lead to a condition called peroneal neuropathy, which is among the most common nerve damage conditions. This damage is typically identified by numbness on the top of the foot and the outer part of the leg, along with an inability to lift the foot properly, also known as foot drop. This results in a distinctive type of walking style called “steppage gait”.
Peroneal neuropathy can be caused by injury, or certain behaviors over time. For example, athletes, or individuals whose job involves a lot of kneeling and squatting are more prone to this injury. This gentle overview should give you a basic understanding of the structure, function, and potential injuries related to the common peroneal nerve.
What Causes Peroneal Nerve Injury?
The peroneal nerve can get damaged due to several reasons, some due to accidents and others not. Some common reasons the peroneal nerve could be damaged include:
* Risk factors related to body structure
* A fibrous band at the start of a muscle near the head of the fibula, a bone in your lower leg, could compress the common peroneal nerve.
* The extensor retinaculum, a ligament that stabilizes the foot is located on top of the ankle. This can squeeze the deep peroneal nerve between it and the bones of the foot, causing a rare condition known as anterior tarsal tunnel syndrome.
A small bone named the fabella, which is found in the calf muscle in about 1% to 30% of people, can press on the common peroneal nerve. This is known as Fabella syndrome.
Accidents or injuries to the knee joint can also cause damage. For instance:
* Dislocation of the knee can injure the common peroneal nerve in up to 40% of patients.
* Direct hits, injuries that break the skin, or cuts can hurt the nerve as it winds around the head of the fibula.
* Breaking the fibula, especially at the upper end.
* Fractures of the tibia, including the tibial plateau.
Outside forces can also compress the nerve, such as:
* Tight splints or casts.
* Compression wraps or bandages.
* Crossing the legs out of habit.
* Long periods of bed rest, even in comatose patients or those on a ventilator for extended periods. During surgery or anesthesia, the way a patient is positioned can lead to compression injury, especially if bony parts like the fibular head are not padded enough.
* Cyst-like tumors or peripheral nerve tumors.
* Accidental damage during surgery on the hip, knee or ankle.
The peroneal nerve is most prone to injury as it winds around the neck of the fibula. This makes it most susceptible to damage at the outer side of the knee.
Severe trauma around the knee could also cause peroneal nerve injury because the nerve is close to the knee joint and superficially located. This could include a direct impact on the fibular neck, cuts, and knee dislocations. Athletes, especially football or soccer players, often suffer from peroneal nerve injuries. In these cases, it’s mostly linked with knee dislocation and damaged ligaments, or these injuries occur in isolation.
Certain widespread illnesses can cause compression of the peroneal nerve and damage to the nerve too, such as:
* Diabetes.
* Inflammatory conditions, like inflammation of multiple nerve sheaths.
* Being exceptionally thin, for example, as a result of anorexia nervosa. Loss of fat beneath the skin can make the nerve more open to compressive damage.
Risk Factors and Frequency for Peroneal Nerve Injury
The peroneal nerve injury is often seen as the most frequent nerve damage in the lower body and the third most overall, surpassed only by the median and ulnar nerves. This type of injury usually happens to young athletes, like football and soccer players, and adults involved in severe accidents like car crashes. It’s reported that between 16% to 40% of patients with knee dislocations can experience peroneal nerve injury. Even overweight people can suffer low-energy knee dislocations during day-to-day activities.
It’s hard to tell the total occurrence of peroneal nerve injuries following closed fractures due to a lack of regularly collected data. However, about 1% to 2% of fractures of the tibia and fibula, bones in the lower leg, may result in peroneal nerve injury. Some cases of nerve injury have also been reported after knee replacement surgery or lateral meniscal repair, although these instances are quite rare. The most noticeable effect of peroneal nerve damage is foot drop, but there’s no data about how commonly this occurs to date.
Signs and Symptoms of Peroneal Nerve Injury
When there is a possibility of injury to the common peroneal nerve (CPN), it is important to conduct a deep assessment of the patient’s history and physical condition. Different factors could influence the type of injury; these could include past knee surgeries, epidural anesthesia, previous knee conditions such as a ‘valgus deformity’, periods of higher body weight, or having diabetes.
The most common symptom of a CPN injury is weakness when lifting the front part of the foot. This is known as ‘foot drop’. It often results in the toes catching on the ground when walking. Sometimes, patients may adopt a style of walking where they lift their feet higher to avoid their toes dragging on the ground. Foot drop can happen suddenly or develop over time, and it can be severe or mild. In some cases, patients might experience numbness or tingling along the side of the leg, top of the foot, and between the big toe and second toe. Pain is sometimes present, particularly in cases of traumatic injury, but not always.
It is crucial to rule out acute damage to the nerves and blood vessels in the knee, which could threaten to compromise the lower extremity in the case of traumatic injuries including knee dislocations. Knee dislocations can seriously affect the nerves and blood vessels running from the thigh and knee to the lower leg. If not treated urgently, this could lead to ‘compartment syndrome’, which may cause lasting damage to the lower leg, possibly even necessitating amputation.
To gauge the involvement of two branches of the CPN – the superficial peroneal nerve (SPN) and the deep peroneal nerve (DPN) – the doctor would examine movements of the foot. If there is weakness in the foot when turning it outwards (eversion) and when flexing the ankle and toes upwards (dorsiflexion), it might suggest an issue involving the CPN. If the injury is closer to the knee, there might be varying degrees of numbness in the areas where the SPN and DPN run.
A common clinical technique called the ‘Tinel sign’ can help identify the location of nerve irritation or entrapment. To conduct this test, the doctor would tap along the path of the nerve, particularly around the area where the fibula (a bone in the lower leg) meets the knee. If tapping triggers a tingling or pins-and-needles feeling further along the nerve from the point of pressure, it is considered a positive Tinel sign.
There are certain tests to briefly assess the motor and sensory functioning of the common peroneal nerve and its branches:
- Motor
- Common peroneal nerve: not applicable
- Superficial peroneal nerve: foot turning outwards
- Deep peroneal nerve: lifting of the foot and big toe upwards
- Sensory
- Common peroneal nerve: the outer side of the leg just below the knee
- Superficial peroneal nerve: the outer lower part of the leg and most of the top of the foot (excluding the area between the big toe and second toe)
- Deep peroneal nerve: the area between the big toe and second toe
Testing for Peroneal Nerve Injury
The Common Peroneal Nerve (CPN) is located near the neck of your fibula (the bone on the outside of your lower leg), and because it’s situated quite close to the surface of your body, it’s particularly likely to get injured. These injuries can come from direct hits or from being compressed by nearby tissues and bones.
If your doctor suspects you’ve injured your CPN, they’ll probably start by ordering plain X-rays. This type of imaging is often the first step in examining the injury. If they need more information, they might also order CT scans (which are more detailed X-rays) to check for any extra bone abnormalities. Additionally, an MRI (which uses magnetic fields and radio waves to create images of your body) or an ultrasound (which uses sound waves to create images) may be used to evaluate any sources or masses in the soft tissue around the injury.
Your doctor might also suggest some tests of your nerve function. These are known as electrodiagnostic studies, and they include electromyography and nerve conduction velocity. These tests study the working and speed of the CPN and its branches. They are particularly useful in locating the exact spot of the nerve injury. These tests are most commonly done in patients who show up with new CPN-related symptoms like foot drop (an inability to lift the front part of the foot), particularly in those patients who didn’t have a traumatic event cause the issue. They may also be used to evaluate patients who have had a surgery due to a traumatic nerve injury to plan their long-term care.
Treatment Options for Peroneal Nerve Injury
There are two main ways to treat CPN (Common Peroneal Nerve) injuries: non-surgical and surgical.
Non-surgical treatments involve using an ankle-foot brace and physical therapy. The brace helps with the bending of toes when walking, provides stability to the ankle, and can even aid in the final part of a step, if needed. Presently, newer foot-ankle braces are made of lightweight carbon fiber, making them more comfortable and efficient during walking or running phases of movement.
When it comes to physical therapy, the treatment will involve various exercises to increase strength and flexibility, improve balance, and improve bodily awareness or ‘proprioception’. Additionally, the treatment may also include wing application on the affected area, using ankle braces, and strapping. There have also been individual cases where ultrasound-guided pulsed radiofrequency treatment helped in relieving the symptoms of nerve entrapment or compression in athletes.
Surgical treatments are usually recommended for fast-progressing nerve injury, if non-surgical treatments show no improvement after three months, or in case of open injuries where the nerve may be cut. Open cuts or wounds should be explored for any nerve damage and treated surgically within 72 hours. Furthermore, patients experiencing bothersome symptoms such as foot drop (where you have difficulty lifting the front part of the foot) due to nerve compression in the leg should know that there’s an option of surgical treatment to relieve the pressure on the nerve, which can be performed with minimal risk.
In some cases of permanent foot drop, muscle-transfer surgery has proven beneficial. If the foot drop is due to muscle tightness, treatment through botulinum toxin injections might be recommended. During surgeries, taking precautions to avoid any CPN injuries is important. This can be achieved by padding the surrounding bony prominences, which include the fibular. The fibular, found on the lateral or outer part of your knee, is often involved in these types of injuries.
What else can Peroneal Nerve Injury be?
Foot drop, a condition where it’s hard to lift the front part of your foot, can be caused by problems in your lower back or in the spot where your sciatic nerve passes through your hip. It’s also commonly due to a specific type of nerve damage known as “CPN neuropathy”. Cases of this type of nerve damage have been reported in people who have undergone hip replacement surgery.
An interesting finding is that foot drop is observed in people with a disorder known as “multiple system atrophy”. This disorder affects several areas of the brain, including those important for movement control. In a particular study, researchers found abnormalities in the action of the muscle responding to a nerve in around 8.6% of patients with a type of multiple system atrophy resembling Parkinson’s disease, and in 4.3% of patients with a kind that seems like a disease called cerebellar ataxia.
What to expect with Peroneal Nerve Injury
The outcome depends on what caused the condition called CPN, or common peroneal nerve, neuropathy. Some mild cases improve or even completely heal over time without needing surgery, but if the CPN is damaged due to a traumatic knee dislocation, it’s less likely to recover fully in the long-term. Quite often, these severe cases may need surgery or tendon transfers, which are decided based on the results of ongoing physical exams and tests that measure the electrical activity and speed of your nerves.
The outcome has been studied in depth in people who injured their CPN during a type of knee surgery called total knee arthroplasty. In one study, 62% of patients had their nerve function mostly return, and 38% had a full recovery by the 12-month mark. Another study that looked at 318 surgically-treated peroneal nerve injuries found that 84% of patients who had their ends of the nerve sewn together experienced a substantial recovery within 24 months.
In patients who needed grafts as part of their treatment, those with grafts smaller than 6 cm recovered 75% of their nerve function. However, longer grafts were linked with worse outcomes.
Possible Complications When Diagnosed with Peroneal Nerve Injury
In patients who have foot drop, it’s important that the medical team, including physical therapy and rehabilitation specialists, incorporate gentle stretching exercises into their treatment plan. These exercises help to prevent a permanent condition known as fixed equinovarus contracture. Specific devices, known as orthotic devices, are also used to make sure the ankle is able to flex upward to a neutral position, even if the patient can’t do it actively.
Common Treatments:
- Passive stretching exercises
- Use of orthotic devices to aid ankle flexibility
Preventing Peroneal Nerve Injury
The healthcare team’s job is to help patients understand the different treatments available for CPN (Common Peroneal Nerve) injuries, including what to expect in terms of healing and potential risks with each option. It is crucial for patients to follow the personal treatment plans made for them, as this tends to lead to the best outcomes.
Patients should also stay in regular touch with their doctor for check-ups and to ensure they’re receiving the right care. In almost all instances, it’s useful for patients to receive clear and positive advice about avoiding issues related to nerve compression, which can happen if you sit with your legs crossed for an extended period of time.